Caring for vulnerable patients during the COVID-19 pandemic
Katherine Ellerby
Katherine Ellerby
RGN, RM, BSc (Hons)
Non-medical independent prescriber, NDFSRH
Practice Nurse, Framlingham Medical Practice, Suffolk & Clinical Research Nurse,
Suffolk Primary Care
With more than two million patients categorised as extremely vulnerable, what should general practice nurses be doing to ensure they are provided with necessary care?
Think back to what working in general practice used to be like before COVID-19. Back to back appointments dominated by patients with significant health needs – the demands on our time and energies felt relentless and we barely had time to catch our breath.
But life has changed. The buzz of a busy surgery with a cramped waiting room has gone, replaced with limited face-to-face consultations in either hot or cold zones, and where the corridors can be eerily quiet as we keep our distance from our colleagues. But our patients, and our patients’ needs, haven’t gone away, especially for our more vulnerable patients. They may be fearful, isolated, anxious. They may not quite know the right thing to do if they become unwell or if they need advice, or help to manage their long term conditions (LTCs). They may feel that the rug of primary healthcare has been pulled from under their feet.
VULNERABLE PATIENTS
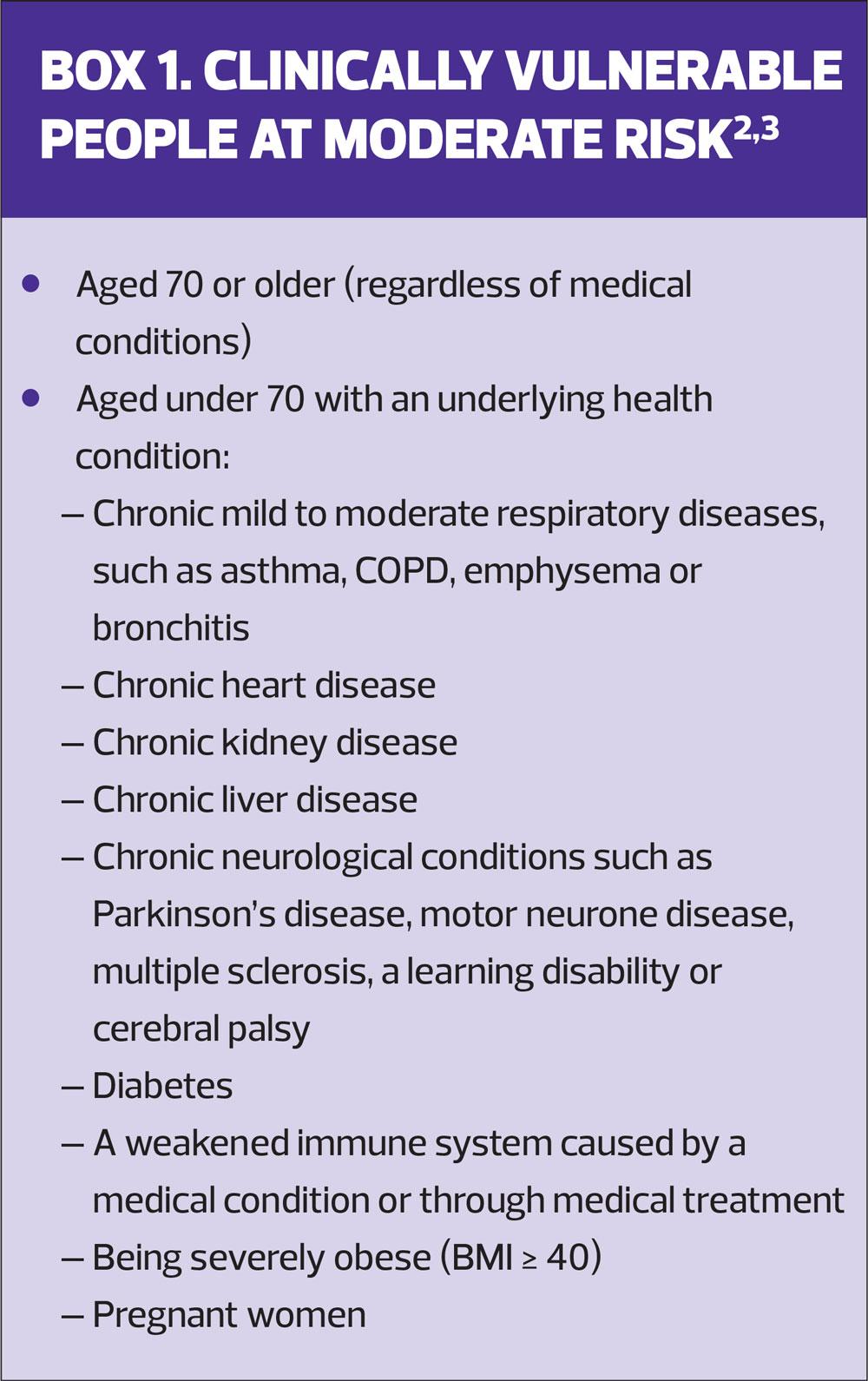
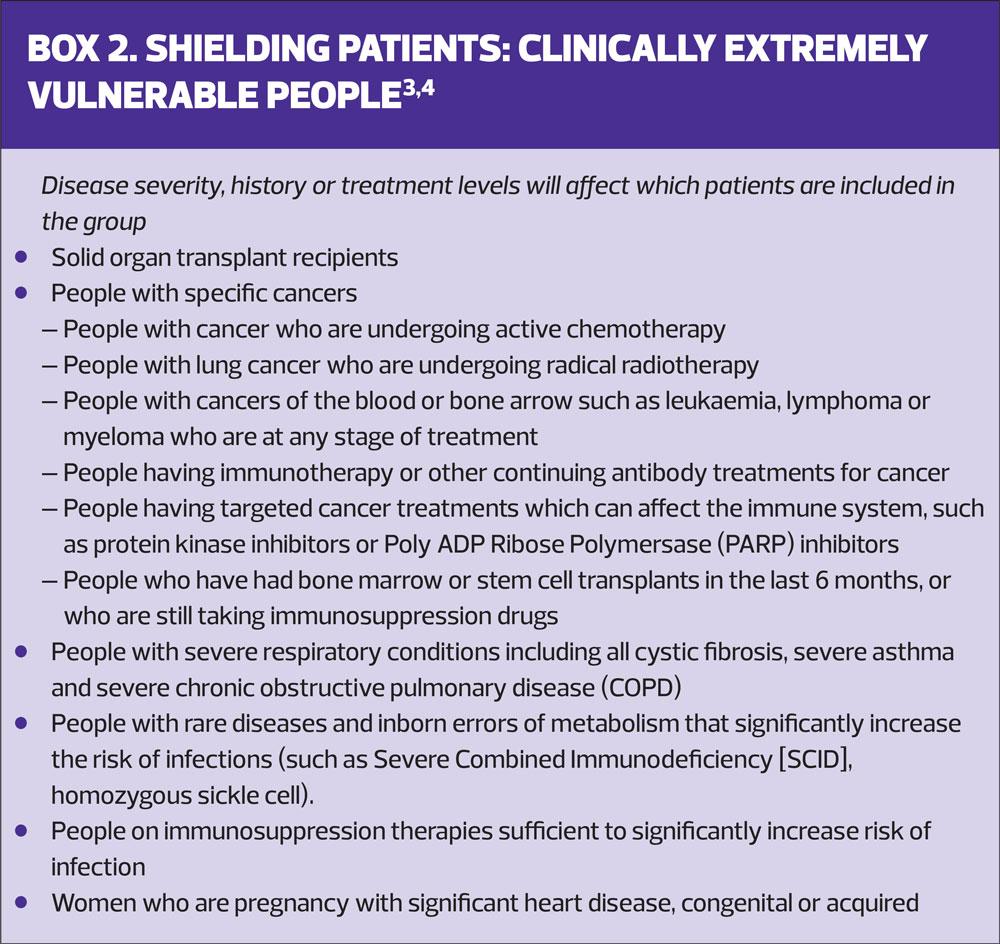
Above all, it is vital that our vulnerable and at risk patients keep safe during this pandemic and avoid risk of infection. We know that COVID-19 has the ability to spread rapidly and extensively.1 We know that the severity of the infection, and risk of critical illness and death, is greater in older patients and those with existing medical conditions but especially those who are clinically extremely vulnerable (Boxes 1 and 2).2-4 Clearly we all have a personal responsibility to reduce our risks of contact and spread of the virus but it is also our professional duty to ensure that our patients, many of whom are extremely vulnerable, are provided with necessary care appropriately and safely.
Shielding extremely vulnerable patients
Patients at the highest risk of severe illness and complications from COVID-19 have been identified via NHS Digital as a priority group.5 Over 2 million shielding patients have been contacted directly by letter and advised of the essential steps they should take to protect themselves, and their carers, from the virus. This list is updated daily and also added to by GPs on a case-by-case basis where patients may have fallen through the net. GPNs can help colleagues identify patients who have missed. Patients have also self-registered with GPs confirming their eligibility.
Shielding means that, for 12 weeks, this group of patients:
- Must not leave their house
- Must not attend any gatherings, including gatherings of friends and families in private spaces (family homes, weddings and religious services)
- Must strictly avoid contact with someone who is displaying signs of COVID-19 (high temperature and/or new continuous cough).
The medical records of patients who are shielding should be clearly flagged so that they can be readily identified by everyone involved in their care.
SUPPORTING PATIENTS WHO ARE SHIELDING
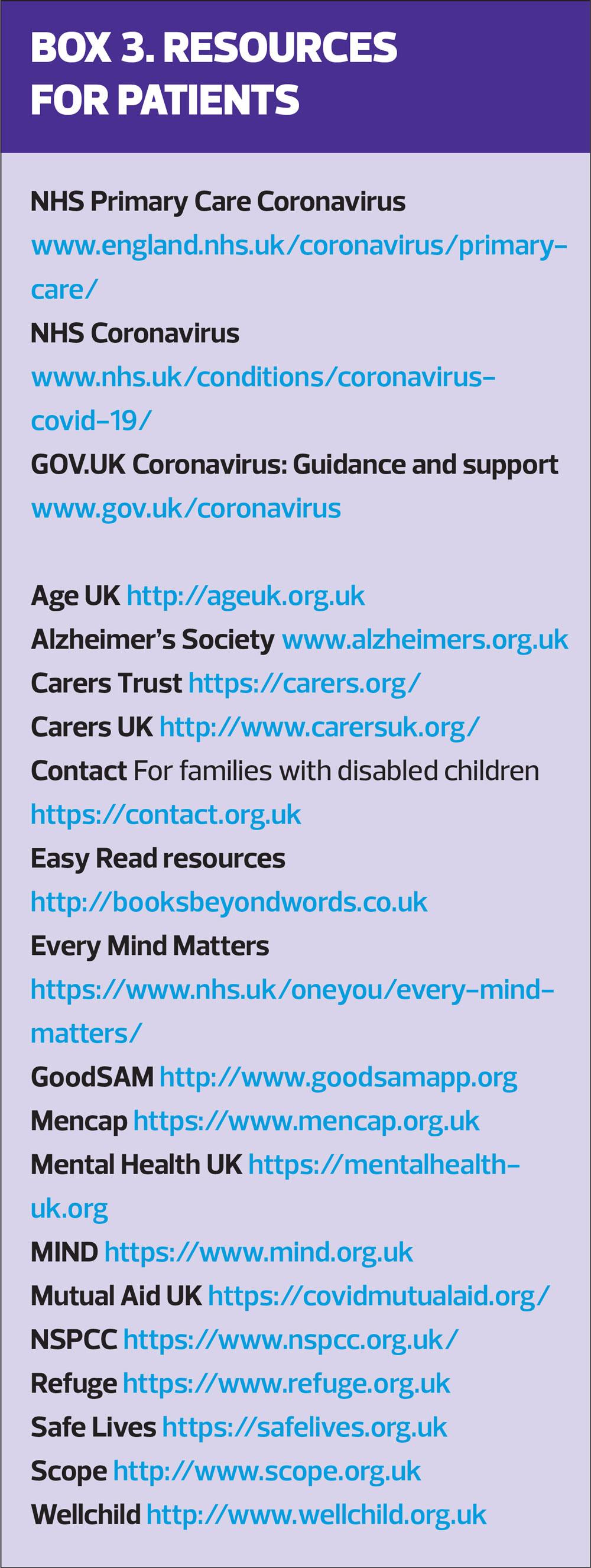
There is a wealth of official guidance for patients who are shielding, including advice on accessing food and medicines, living safely with other people, making plans and back-up plans for essential carers as well as advice about looking after emotional wellbeing, keeping physically active and staying connected with family and friends (Box 3).4 We should be contacting these vulnerable patients, by phone or video link, checking they understand what shielding means and how it relates to their personal circumstances, ensuring they can access their medications and address any urgent or ongoing health needs or concerns they have. They may need signposting to local community volunteers or good neighbourhood schemes, to the NHS Voluntary Responders Programme or social prescribing link workers.
Many patients may be reluctant to contact their practice for fear of ‘troubling’ a highly publicised overstretched NHS. There may be patients out there who feel that their health needs now take second place to patients with COVID-19. But we have an essential role in identifying the worsening of any long term conditions, albeit remotely, and treating any acute illness in our high risk patients to reduce hospitalisations and prevent morbidity and mortality from non-coronavirus causes.
HOME VISITS
Shielded patients should not be attending the surgery but if any consultation needs to be carried out face-to-face, then these patients may require a home visit by the most appropriate health professional for that individual need and in line with the specific infection prevention and control guidance.1 GPNs visiting shielded patients need to ensure for each visit they:
- Have ‘home visit’ bags with appropriate PPE and clinical waste disposal
- Carry out thorough hand-washing before, during and after direct patient care and after removal of PPE – ideally with soap and water or, if not possible, with alcohol gel
- Double bag any waste items which have been in contact with the patient, tied and set aside for 72 hours before disposal as per local policy
- Be aware of items which may be potentially carry a risk of cross-infection e.g. pool car, mobile phone, pens etc
- Work in line with local policy for lone working
GPNs should segregate any home visits to either patients with no COVID-19 symptoms OR those with symptoms (including household members). If this is not possible, then the priority must be to see patients without symptoms first.6 Any home visits undertaken by GPNs must be deemed absolutely essential and only done if there is no alternative.
NON-SHIELDING VULNERABLE PATIENTS
We also have many patients who are still vulnerable but who don’t fit the criteria for shielding. Vulnerability also applies to our frail elderly population, and patients with learning disabilities and special needs, and their carers. Furthermore, from a safeguarding perspective, we must exercise particular vigilance in recognising the greater risks for vulnerable individuals and families at this time.
Elderly patients
Keeping our elderly patients safe and well during this time of social distancing is so important. Online resources such as the NHS website and Age UK have helpful suggestions for:
- Staying safe
- Maintaining physical and mental wellbeing
- Managing anxiety surrounding the pandemic
- Using technology for social interaction
- Keeping occupied with activities and hobbies
Our elderly patients may need to be reassured they have the same access to GP services as before, albeit virtually. From an LTC perspective it means we need to prioritise those at greater risk – for example, those with poorly controlled diabetes and patients with COPD or asthma with frequent exacerbations and/or hospitalisation while routine annual reviews are carried out by telephone or put on hold.
Patients may need advice about the risks of dehydration with specific medications, e.g. diuretics, ACE inhibitors, metformin and long term NSAIDs, if they become unwell and to seek medical advice accordingly. We also need to consider the frail elderly, who are at greater risk of hospital admissions, who we need to keep tabs on and ensure they have support in place.
Carers of people with dementia may find dealing with the restrictions and hygiene measures an additional burden. We can make contact with this group to ensure they have access to the support and resources they need. Furthermore, carers need to be aware of the increased risk of delirium with infection for people with dementia, how to recognise the signs, and to seek medical help early.
Special needs and care provision
Adults and children with special needs and disabilities may be reliant on other people to assist them in their daily lives. It is imperative that caregivers – whether a family member, friend, neighbour or a paid carer – continue to provide essential care as long as they take the correct precautions and also as long as they, or someone in their household, do not have symptoms of coronavirus.1,7 Whilst there is an increase in the need for caregivers at this time, care provision is also threatened as fewer people are able to fulfil their role as they themselves become unwell or have to self-isolate. This can be very frightening for families worried about the threat to their support network. Ensuring contingency plans are in place is absolutely vital, especially as carers may have to cancel at short notice. These plans need to be readily accessible so they can be implemented before a crisis occurs. See Caring for carers Practice Nurse April 2020;50(4):24-28. Charities and volunteer support groups, such as Scope, WellChild, Covid-19 Mutual Aid are helping to address this balance to provide practical help in addition to local schemes.
Learning disabilities and autism
We need to ensure that people with learning disabilities (LD) and autism are adequately supported during this pandemic. Much of their face-to-face support will have been withdrawn due to the social distancing measures leaving them more vulnerable. Instead, voluntary and community support may be accessible virtually via social media outreach and listening support. GPNs can liaise with link workers to ensure that our LD registers correspond with the social care registers to identify all the people that require help. People with LD may need additional support to understand why changes to daily routines and behaviours are necessary. There is a potentially greater risk of infection for people with learning disabilities due to their personal habits. Easy read guides and videos on social distancing, hand-washing and facts about COVID-19 are available to support people with LD and autism at https://www.mencap.org.uk/advice-and-support/coronavirus-covid-19 (Box 3).
Domestic abuse
Until 10 May* the advice was to stay at home, save lives. But what if your life feels threatened not so much by the risk of coronavirus itself, but by having to stay at home? Being trapped in a home environment, with a partner who is no longer going out to work, controlling every move, being verbally, physically and/or emotionally abusive, cut off from the lifeline of family, friends and community can be terrifying. Financial anxieties, excess alcohol consumption and fears surrounding the pandemic can all serve to intensify feelings of fear and isolation. Reporting of domestic abuse has increased since lockdown.8 Support services for victims of domestic abuse are working quickly to ensure help remains available and helplines and online resources are providing COVID-19-specific guidance for people at risk of, and subject to, abuse. People suffering domestic abuse are not constrained by the home isolation directive if they need to escape their home.9
*On 10 May Prime Minister Boris Johnson changed the official advice from 'Stay home, Protect the NHS, Save lives' to 'Stay alert, Control the virus, Save lives'
Safeguarding
At times of crisis, we see the best, but also the worst of humankind. On one hand you have communities pulling together to ensure those in greater need are looked after. On the other, there are unscrupulous people who take advantage of the pandemic and prey on people who are more vulnerable, more dependent – and more at risk. Carers may also snap under the pressure, and take it out on those they are caring for. Those at greatest risk are people who have care and support needs, who are less able to protect themselves and are experiencing, or are at risk of, abuse or neglect.10
We need to be vigilant for signs of abuse through nuances of behaviour change or the tone of voice when speaking to our patients on the phone. We can also ask direct questions about who else is in the house, if it is safe to talk, and if they feel safe.11 We should know who the most vulnerable and isolated patients are in our practices and check in with them to ensure their wellbeing. Liaising with our link workers, we should also know which of our families are at risk. The impact of intense financial hardship, social isolation and lack of face-to-face contact puts these families at even greater risk. As we continue with routine childhood immunisations, we still have opportunities and responsibilities to identify any safeguarding concerns. And while there may be a reduction in routine local authority services at this time, urgent and serious care needs must still be met and our duty of care to our patients who may be at risk of serious harm or neglect is paramount.
MENTAL AND EMOTIONAL WELLBEING
We cannot underestimate the huge impact COVID-19 has had on people’s emotional wellbeing whether they have existing mental health problems or not. Patients unable to leave the house may feel intensely isolated and lonely. Without face-to-face contact many people are struggling to get through each day. Our vulnerable patients can be referred to the Royal Voluntary Service to ‘check in and chat’ with one of the NHS Volunteers, and we should be encouraging our patients to take just one day at a time.12,13 Every Mind Matters and the NHS app have plenty of top tips to help people to look after their mental health, from encouraging people to talk about their worries, to what local support is available, and limiting their exposure to media coverage of the outbreak.
Our vulnerable patients were there before COVID-19 but now more than ever, we need to make sure that they are not temporarily lost because of it.
REFERENCES
1. Public Health England. Covid-19: Infection prevention control guidance. Last updated 27 April 2020. https://www.gov.uk/government/publications/wuhan-novel-coronavirus-infection-prevention-and-control
2. Gov UK Guidance: Staying at home and away from others. Last updated 1 May 2020.
3. NHS Digital. Coronavirus (COVID-19) Shielded patients list. https://digital.nhs.uk/coronavirus/shielded-patient-list#latest-news
4. Public Health England. Guidance on shielding and protecting people who are clinically extremely vulnerable from COVID-19. Updated 5 May 2020.
5. NHS Digital. Shielded patients list: guidance for General Practice. https://digital.nhs.uk/coronavirus/shielded-patient-list/guidance-for-general-practice
6. NHS. Novel Coronavirus (COVID-19) standard operating procedure: Community Health Services. 15 April 2020. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/04/C0198-community-health-services-sop.pdf
7. Department of Health and Social Care: Guidance for those who provide unpaid care to friends or family. 8 April 2020. https://www.gov.uk/government/publications/coronavirus-covid-19-providing-unpaid-care/
8. Social Care Institute for Excellence. Domestic violence and abuse. Safeguarding during the COVID-19 crisis. 22 April 2020. https://www.scie.org.uk/care-providers/coronavirus-covid-19/safeguarding/domestic-violence-abuse
9. Home Office. Guidance. Coronavirus (COVID-19): support for victims of domestic abuse. 14 April 2020.
10. Social Care Institute for Excellence. Safeguarding adults during the COVID-19 crisis. Updated 1 April 2020.
11. RCGP Learning Top Tips. Covid 19 and Safeguarding: Practical tips for safeguarding children, families and vulnerable adults during this period. Last modified 7 May 2020. https://elearning.rcgp.org.uk/mod/page/view.php?id=10552
12. NHS. Every mind matters. https://www.nhs.uk/oneyou/every-mind-matters/
13. Public Health England. Guidance for the public on mental health and wellbeing aspects of coronavirus (COVID-19); Updated 31 March 2020.
Related articles
View all Articles