Managing the vaccine fridge
Maintaining the cold chain is critically important in ensuring vaccine efficacy and therefore underpins the entire public health immunisation programme
The surgery has three vaccine fridges. Childhood vaccines are stored in one, and the other two are used for travel and adult vaccines. On Monday morning, after a hot weekend and with a full childhood immunisation clinic booked, you check the fridge containing the childhood vaccines and the temperature readings are +11°C maximum, and +9°C minimum. The average reading is +10°C. The last readings were on Friday evening and were within the normal range. It is at this point you notice the fridge has been switched off at the socket. What should you do?
Vaccines are biological substances; the efficacy of vaccines will naturally deteriorate, and if stored outside the recommended temperature range this process maybe accelerated.1 Once the vaccine effectiveness is reduced it cannot be restored.1 Inappropriate transportation and storage of vaccines may result in reduced efficacy of the vaccine, lower immune response and poor protection against disease.2
Maintaining the cold chain is therefore a key factor in preventing and eradicating many common vaccine-preventable diseases globally.3 The ‘cold chain’ means maintaining the safe transportation and storage of vaccines within the recommended temperature range of +2°C to +8°C, from production to administration to the patient.1
Each vaccine has a different vaccine stability, some are more susceptible to heat and others to cold.1 Inactivated vaccines tend to be more sensitive to freezing; this is because they often contain aluminium-based adjuvants (which can be destroyed by freezing) to prime the immune system.3 Freezing of a vaccine may lead to deterioration of the content and may also cause hairline cracks in the vial or prefilled syringe which could contaminate the ingredients.1 Live attenuated vaccines generally tend to be more susceptible to heat, as are freeze-dried preparations following reconstitution.1 If a live vaccine is reconstituted and not used immediately, the summary of product characteristics (SPC) will give guidance on how long a it may be stored.4 All vaccines should remain in the original packaging to maintain a constant temperature and protect against exposure to natural and strong artificial light, as this can affect the potency of some vaccines, such as bacillus calmette-guerin (BCG), measles, mumps and rubella (MMR), varicella and most diphtheria, tetanus, acellular pertussis (DTaP)-containing vaccines.3 All vaccines should be stored according to the manufacturer’s instructions as outlined in the SPC.1
Vaccine wastage is still a significant financial loss to the NHS: in 2017 it was estimated £5 million was wasted due to breaches in the cold chain.5 Even a small reduction in vaccines wastage would have a major, positive impact.
HCPs are pivotal to ensuring patients are offered optimal protection against vaccine preventable diseases. All staff involved with immunisation programmes are responsible for maintaining the cold chain, and should be appropriately trained to ensure the cold chain compliance.1
The Green Book provides guidance on the minimum standards expected of all staff involved with immunisation,1 backed up by additional country-specific guidance from Public Health England, Health Protection Scotland, Public Health Wales, and Northern Ireland Health and Social Care Board. These resources may vary in some respects, so follow your own national guidance.6
The national standards recommend your work-based protocol should include guidance on:7
- Ordering and delivery
- Storage of vaccine
- Maintenance of the cold chain
- Monitoring and auditing of stock levels
- Incident reporting
VACCINE STORAGE
All clinical settings must have a validated vaccine fridge specially designed for pharmaceutical products, placed in a well-ventilated area away from direct heat sources and out of direct sunlight. Fridges should be calibrated every 12 months. Accidental interruption of the power supply is a common reason for breach in the cold chain.8 The UK standards recommend having a switchless socket for vaccine fridges or clearly label the plug, ‘do not switch off’ and to have back up facilities in place in the event of fridge failure. It is preferable to have two thermometers, one with an independent source so it there is an interruption of electricity supply, temperature readings can still be obtained. Use of a data logger can be helpful: they are relatively cheap to buy, and provide continuous computerised readings that can be used to identify exactly when any cold chain breach occurred.5
The recommended temperature range is +2°C and +8°C (average reading +5°C). As all vaccines are prescription only medicines, they should be stored in a locked fridge or locked room.1 Fridge capacity should be adequate for storage of all vaccines, including additional stock for busy periods i.e the flu season.1 This is to allow air to circulate and maintain a constant temperature. It is good practice to have designated areas for different vaccines in the fridge for easy access and to reduce the length of time the door is open, to avoid temperature fluctuations.1
Fridge temperatures must be recorded and documented at least once every working day. It is good practice to record the temperature readings at the start and end of each working day.3 Temperature records and a full vaccine inventory should be retained for at least one year but it is good practice to keep comprehensive records for 5 years as some vaccines have a shelf life for 4 years or longer.1
When delivering a vaccine programme in outlying clinics or on domiciliary visits, it is essential to transport vaccines in a validated cool box, recording its temperature at the start and end of the session.1
ORDERING VACCINES
The vaccines for the routine immunisation programmes are provided centrally. Stock levels should not exceed more than 2 to 4 weeks’ supply. Order small quantities of vaccines on a regular basis and ensure there is adequate vaccine supplies to meet the clinical need. Check stock levels regularly to avoid any under- or over-ordering. The practice’s nominated person (or deputy) should check delivery of all vaccine orders for any inconsistencies and/or damaged items. On receipt, vaccines should be refrigerated immediately.8
STOCK ROTATION
Regularly rotate stock as the most recent vaccine delivery may not have the longest shelf life. Vaccines with the shortest expiry dates should be used first, as those approaching the end of their shelf life are more vulnerable to deterioration.6
A robust system should be in place to monitor vaccine orders, expiry dates and maintain an ongoing total of vaccines including any vaccine wastage. Stock levels should be checked and updated at least once a month. Vaccines should be stored away from the sides and back of the fridge, which may cause them to freeze and become ineffective.8
IF THERE IS A BREACH IN THE COLD CHAIN
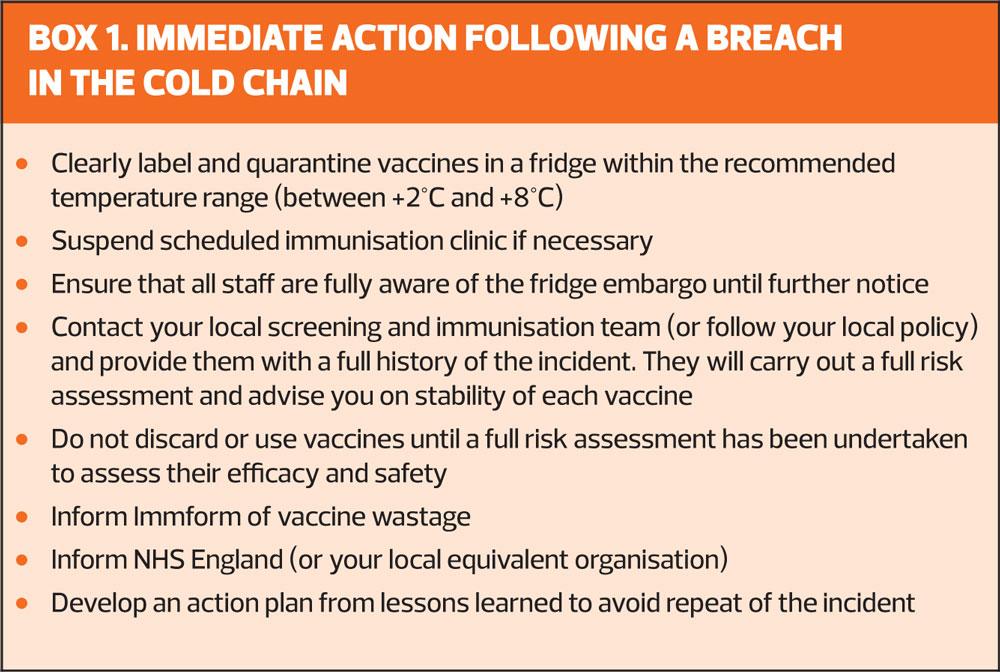
If, as in the opening scenario, there is a fridge failure leading to a breach in the cold chain, follow the immediate actions set out in Box 1.
You may need to suspend planned immunisation clinics until the local screening and immunisation team has completed a full risk assessment. You will need to provide a full history of the incident, and details of any patients who have been vaccinated inadvertently with an affected vaccine.
The team will advise you about each vaccine’s stability, and which – if any – are still safe and effective to use.8 Any that are deemed suitable for use will be classed as off-label (because the storage guidance in the product license has not been followed). As such, they will no longer be covered by a patient group direction, but can still be administered under a patient specific direction.9 When giving any off-license medicinal product, the patient (or carer) should be informed and the decision to proceed recorded in the medical record.10
LESSONS LEARNT
When there is a breach in the cold chain it is important as an organisation to learn from the incident. Significant event analysis (SEA) should act as a learning process for the whole team. It is essential to reflect from the incident and develop an action plan to avoid it happening again and to continue to improve patient care.11
CONCLUSION
To have a successful immunisation programme it is essential to maintain the correct temperature range for the safe transportation and storage of vaccines. The immuniser needs to ensure the cold chain has been maintained to offer optimal protection for patients against vaccine-preventable diseases.
REFERENCES
1. Public Health England. Storage, distribution and disposal of vaccines: The Green Book, chapter 3, 2013
2. Center for Diseases Control (CDC). Vaccine Handling and Storage Toolkit 3 January 2019
https://www.cdc.gov/vaccines/hcp/admin/storage/toolkit/storage-handling-toolkit.pdf
3. WHO. The vaccine cold chain. Module 2. https://www.who.int/immunization/documents/IIP2015_Module2.pdf
4. Electronic Medicines Compendium https://www.medicines.org.uk/emc/
5. Public Health England: Vaccine Update: issue 294 January 2018 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/680798/Vaccine_Update_274_January_2018_.pdf
6. Chiodini J. Safe storage and handling of vaccines Nursing Standard 2013; December: 45 – 52 https://www.janechiodini.co.uk/wp-content/uploads/2017/07/Safe-Storage-and-Handling-of-Vaccines-Nursing-Standard.pdf
7. Public Health England. Protocol for ordering, storing and handling vaccine, March 2014 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/300304/Protocol_for_ordering__storing_and_handling_vaccines_March_2014.pdf
8. Health Protection Agency. Vaccine Incident Guidance: responding to vaccine errors, April 2014 https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/326417/Vaccine_Incident_Guidance.pdf
9. NHS England South West, Patient Specific Directions: April 2016. https://www.england.nhs.uk/south/wp-content/uploads/sites/6/2016/09/patient-specific-directions.pdf
10. General Medical Council: Ethical guidance: Prescribing unlicensed medicines
11. Care Quality Commission. Nigel’s surgery 3 Significant Events Analysis: August 2017 https://www.cqc.org.uk/guidance-providers/gps/nigels-surgery-3-significant-event-analysis-sea