Upskilling healthcare assistants to ease diabetes review workload
Louise Dale
Louise Dale
RGN, MSc, NMP
Practice nurse, Pickering, North Yorkshire
Practice Nurse 2020;50(9):21-24
Facing increasing challenges in ensuring that our growing number of patients with diabetes received the full range of health checks in a timely way, we launched an initiative to increase the skill set of healthcare assistants – and to improve nurse availability for diabetes reviews
The pressures of an ageing population, the need for better health outcomes, recruitment and retention issues all present appointment capacity challenges for primary care. In addition to these factors, Diabetes UK estimates that the known numbers of people with diabetes has risen by 60% in the last decade.1 To manage the challenge of limited appointment availability, coupled with the burgeoning diabetes register, innovative changes are needed to allow patients living with diabetes to be seen as planned for their diabetes annual reviews without compromising patient safety.
THE PROBLEM
Our semi-rural practice, which participates in a Quality Improvement Project (QIP), has two diabetes nurses who manage 718 patients with diabetes on the Quality and Outcomes Framework (QOF) register. The practice, at the time of the project, was served by five Health Care Assistants (HCAs). Waiting times to see a HCA were 0 days in comparison to a wait of up to 4 weeks to see a diabetes nurse. Patients with diabetes at the practice are invited to be seen in their birthday month, however many patients had not been seen until the following month due to availability of appointments with a diabetes nurse.
MAKING THE MOST OF HCAs
HCAs have the potential to improve capacity and efficiency in general practice, and their role has expanded with developments in training to underpin this objective.2 They are immensely valuable members of the primary care team, and work successfully to protocols. However, they are not expected to make clinical judgements.
Previously, the HCAs performed a blood test, measured blood pressure, height, and weight and also discussed alcohol intake and smoking history, all in preparation for the patient’s appointment with the diabetes nurse. We proposed to train HCAs to also perform foot checks during the HCA appointment in addition to their current tasks. The purpose of this change was not only to upskill the HCA team, but to use their free appointments and to ensure that patients on the diabetes register would not have to wait as long to see a diabetes nurse, thus decreasing the workload in the annual review appointment and therefore reducing waiting times to see the diabetes nurse. We calculated that it would allow for two further appointments to be added for each 4.5 hour clinic. The HCAs would receive a further 10 minutes to complete their previous observations and also complete a thorough foot assessment, escalating any concerns following a rigid protocol.
NICE guidance recommends that people with diabetes have regular foot assessments by a health care professional.3 This review includes an examination of the feet and footwear, checking for deformity, pulses and sensation, classifying foot risk and promoting good foot care. NICE guidance doesn’t, however, stipulate which health care professional should be assessing patients’ feet as part of the diabetes review, providing the individual has received adequate training.
Of course, there are key issues when expanding the scope of practice of HCAs. Nurses must ensure that the care they delegate is within the competence of the individual accepting the task. Equally the registered nurse and HCAs have a duty of care and are accountable to the law, and must work to protocol.4 All staff must perform skills competently; take accountability for accepting the delegated skill; understand the skill and work in the best interests of the patien; and inform the registered nurse if they have any concerns around delegation.4
TRAINING
A study day was designed for HCAs to develop their skills and knowledge in diabetic foot care. Participants included all five HCAs working at the practice at that time. The HCAs attending the study day had differing levels of ability and educational background, with some possessing no formal qualifications, although many had tacit knowledge and experience. This is in contrast to many nursing students who have acquired theoretical knowledge to support their practice but may lack the practical experience to appreciate its application. The training used an established online training resource (http://www.diabetesframe.org/
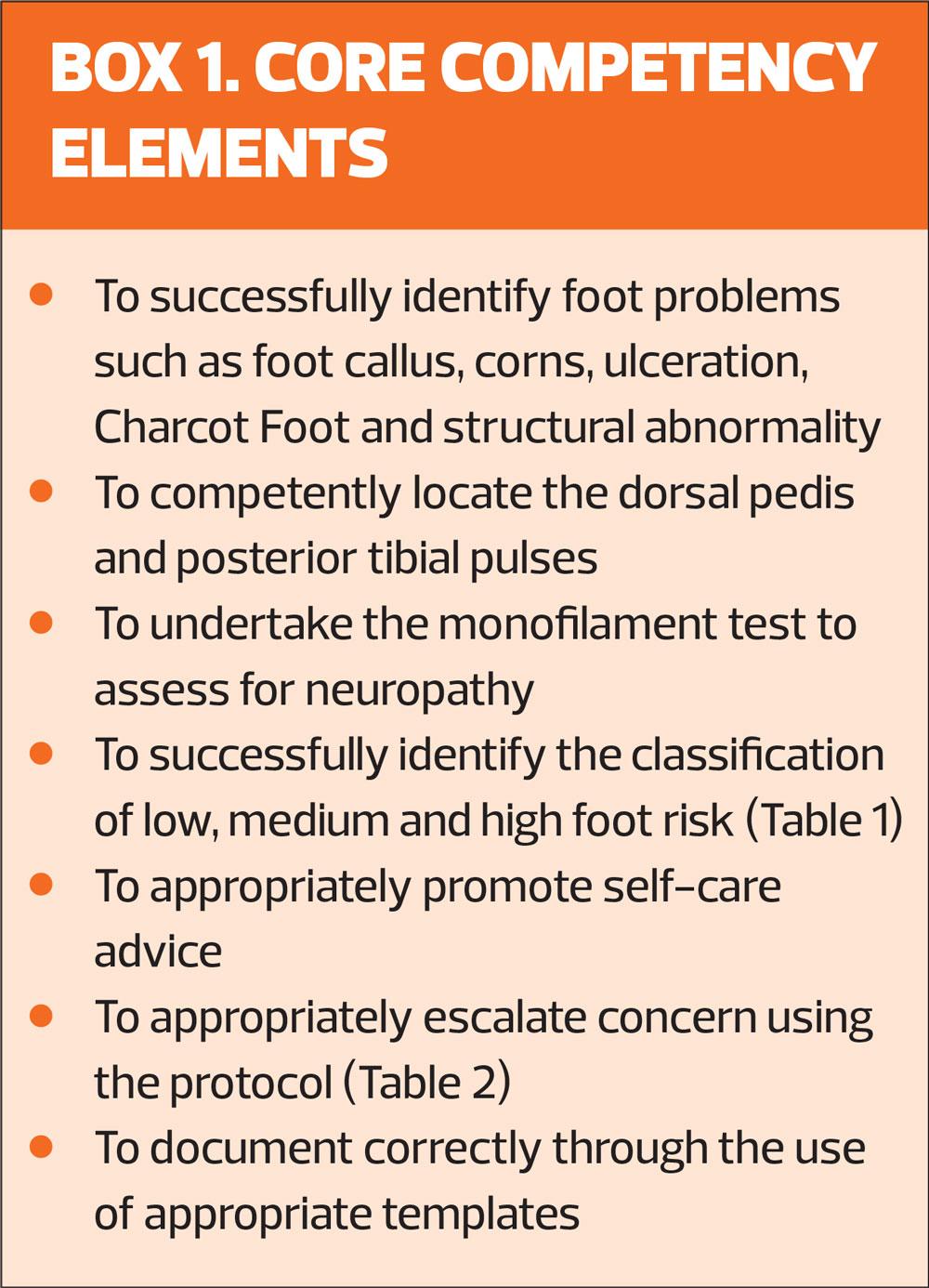
training.asp)5 and a face-to-face training session including practical training. The trainees completed a competency framework to assess their confidence, competence and knowledge, (Box 1) and feedback was obtained to highlight future learning needs.
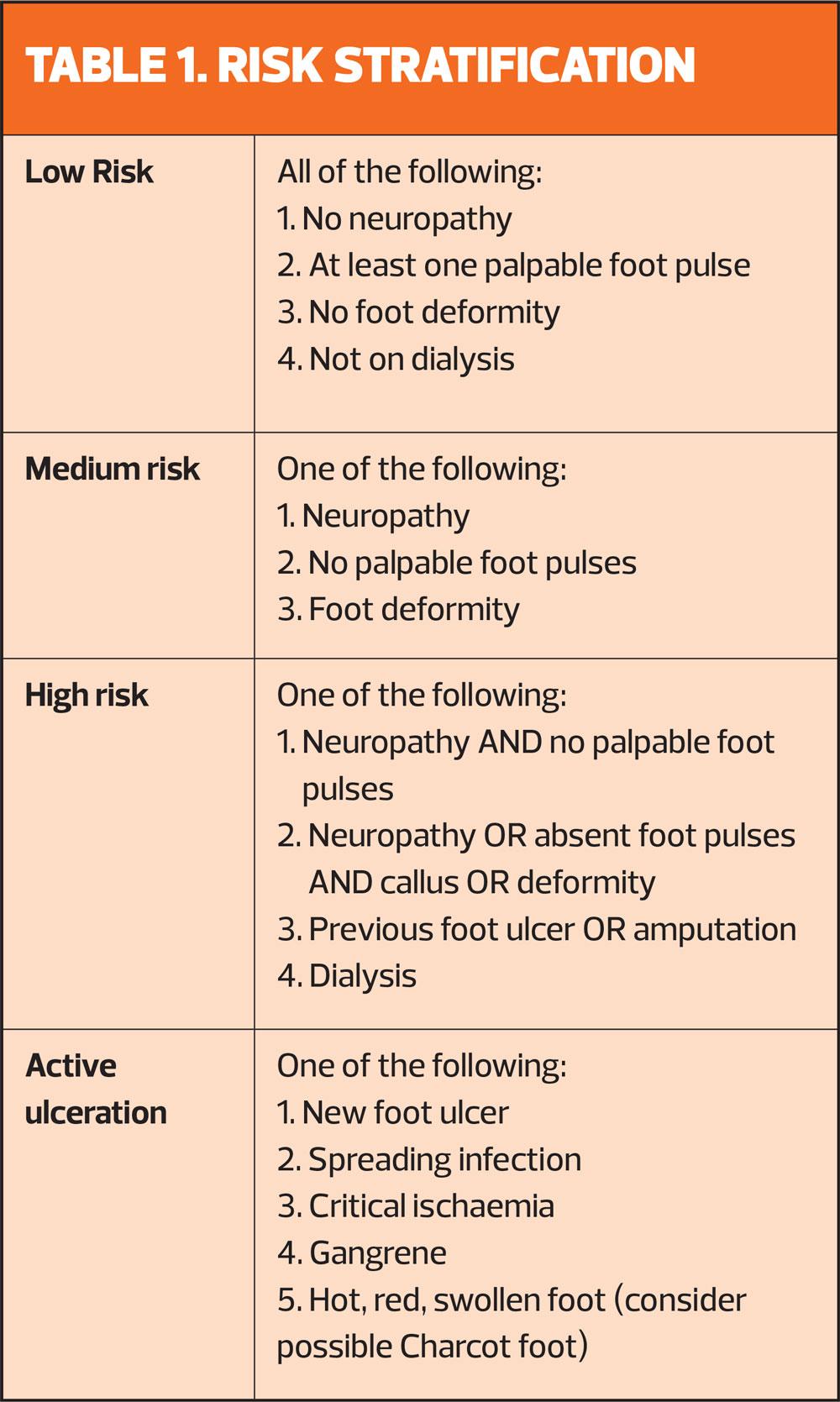
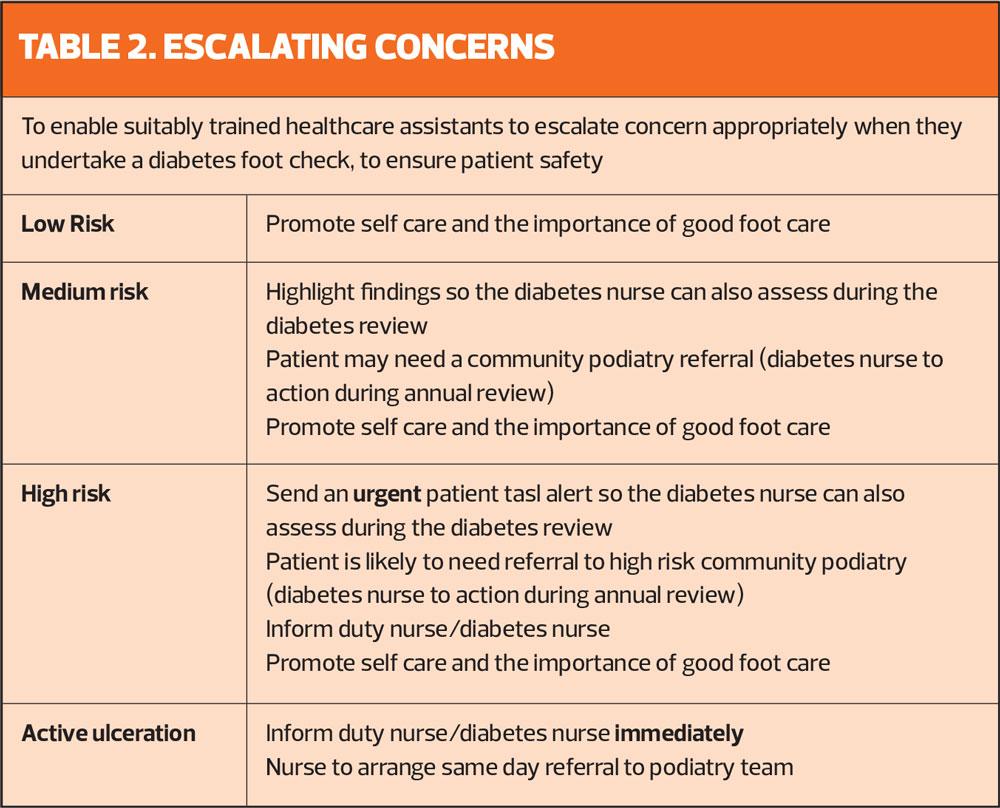
A requirement during the foot assessment is to classify the risk of foot complications in each individual. A protocol is available locally which classifies patients risk based on foot sensation and palpable pulses. To ensure patient safety, an ‘escalating concern flow chart’ was produced for the HCAs, based on the protocol, to inform key members of staff immediately should the patient have active ulceration or any worrying foot problems that would be outside the remit of the HCA.
FEEDBACK AND ONGOING REVIEW
A feedback form was completed by each HCA one month after the improvement project had begun: feedback was mostly excellent. Comments included, ‘The more I do, the more confident I am;’ ‘I always feel that I can approach the diabetic team for support;’ ‘Doing foot checks is another skill and it is fantastic that I feel competent.’
There were a few teething troubles with appointment times – some patients continued to have 10 minutes appointments with a HCA followed by 30 minutes with a nurse – but the impact was minimal, as the error was mostly picked up by the receptionists when booking the appointments. An informal oversight of appointment booking was done remotely at the 2 month stage and all patients had appropriate appointment times.
Following skill acquisition, regular reviews of competency need to be carried out to ensure safe practice is maintained.6 ‘Spot checks’ were carried out 3 months after the initiative was underway to cross check the HCA’s assessment with the diabetes nurses’ assessments.
RESULTS AND LIMITATIONS
Five months after the launch of the initiative, waiting times were analysed again. The waiting time to see a diabetes nurse had reduced to 2 weeks, or even less when no one was on annual leave.
One limitation highlighted by both nurses was that having a full clinic with 20 minutes per patient proved difficult if not all reviews were straightforward. Some patients had complex histories, required further lifestyle advice or some patients needed their medication to be increased or changed. To overcome this problem, the nurses requested two ‘catch up time’ slots to be added to help the nurses continue to run their clinics to time.
CONCLUSION
Since the introduction of this project the waiting time for nurse appointments for patients with diabetes has improved by 50%. In reality this achievement could be greater in the periods where no annual leave is taken. The HCAs have proven to be champions of their new skill, enthusiastic and they are driving this initiative forward, proving its success. Of course, the HCA role will always have limits, nevertheless with appropriate training, support, competencies and protocols, their role can continue to develop. There may be some overlap between registered nurses and HCAs, in the same way as the gap tends to be closing between the roles of the practice nurse, nurse practitioner and general practitioner. However, it is fundamental to have clear boundaries, appropriate competence-based training, protocols and a thorough understanding of accountability and delegation and this quality improvement project reflects these standards.
REFERENCES
1. Diabetes UK (2015) 60% increase in last decade. www. diabetes.org.uk/about_us/news/diabetes-up-60-per-cent-inlast-decade-/ (accessed 10 September 2019)
2. Kessler I, Heron P, Dopson S. The Modernization of the Nursing Workforce: Valuing the Healthcare Assistant. 2019; Oxford: Oxford University Press
3. NICE NG19. Diabetic foot problems: prevention and management; 2015 www.nice.org.uk/guidance/ng19
4. Royal College of Nursing. Accountability and delegation: what you need to know. The principles of accountability and delegation for nurses, students, health care assistants and assistant practitioners; 2017. https://www.rcn.org.uk/professional-development/accountability-and-delegation
5. Foot Risk Awarenessness and Management Education (FRAME). Diabetes Foot Screening. http://www.diabetesframe.org/training.asp
6. Nursing & Midwifery Council. The Code. Professional standards of practice and behaviour for nurses, midwives and nursing associates; 2015 (updated 2018). https://www.nmc.org.uk/standards/code/