Practice Nurse Bite-Sized LearningUnderstanding Atrial Fibrillation
Joanne Haws RN MSC, Clinical director, Learn with Nurses
Joanne Haws RN MSC, Clinical director, Learn with Nurses
Michaela Nuttall
RGN MSc, Founder & Director, Learn with Nurses
Practice Nurse 2023;53(5):10
INTRODUCTION
Atrial fibrillation (AF) is the most common cardiac arrhythmia, with around 1.5 million people in the UK living with the condition.1
WHAT’S THE PROBLEM?
AF is an atrial tachyarrhythmia characterised by predominantly uncoordinated atrial activation with consequent deterioration of atrial mechanical function.2 If undetected, or left untreated, AF is a significant risk factor for stroke and other morbidities. The risk of stroke is increased five-fold in those with AF and these are often very severe and disabling strokes.3
DETECTION
Many people with AF do not experience symptoms, though some report palpitations, dizziness or other symptoms.4 To reduce stroke risk, it is essential that AF is found through case finding and opportunistic pulse checks. The risk of AF increases with advancing age and in those with or at risk of CVD, therefore most cases will be found in these groups.5
DIAGNOSIS
To detect AF the radial pulse should be palpated for 60 seconds and if this is found to be irregular a 12-lead echocardiogram (ECG) should be performed. Where AF is paroxysmal (comes and goes) it may easily be missed, and other recording devices may be more helpful – such as handheld single lead ECG monitors or longer periods of recording.6
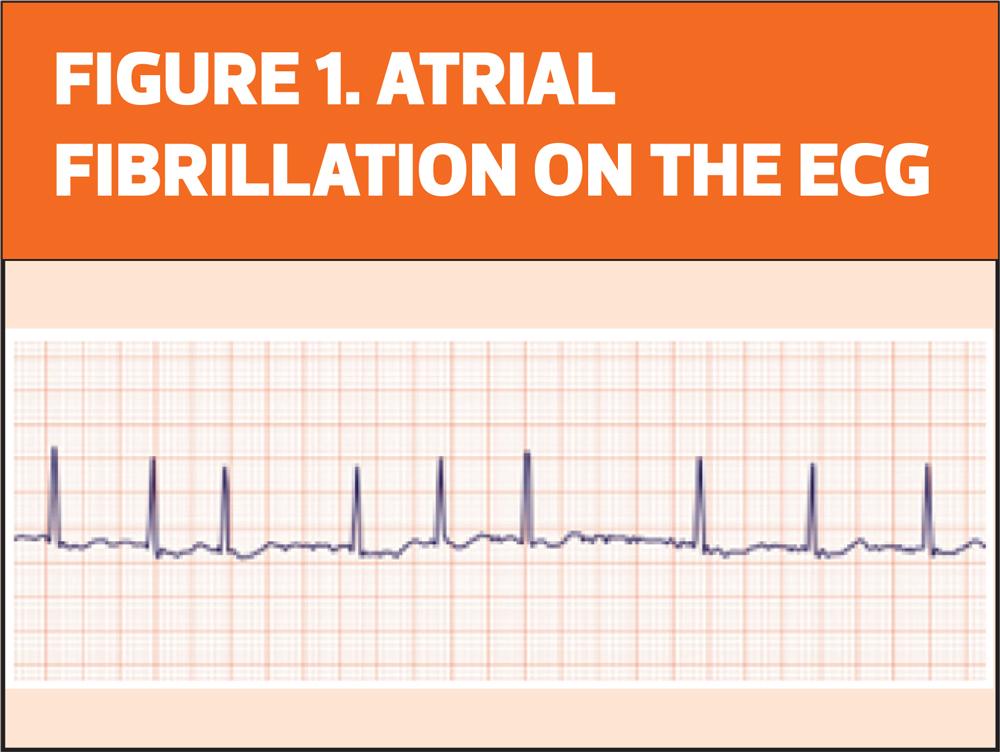
On the ECG showing atrial fibrillation (Figure 1) you will see:
- Lack of visible P-waves
- A fibrillating baseline
- Irregularly irregular QRS complexes
- A variable ventricular rate
MANAGEMENT
Treatment of the arrhythmia will be dependent of the classification of the AF, whether it is paroxysmal, persistent or permanent, and will either be a rate or rhythm control strategy.
The rate strategy focuses on managing the heart rate to a level that reduces symptoms and minimises reduction in cardiac output.6 The aim is to slow down the heart rate until either a resting heart rate of <110bpm AND without symptoms is achieved, or HR<85bpm in those with ongoing symptoms.
The rhythm strategy aims to restore normal sinus rhythm.
Regardless of the management of the arrhythmia itself, a key focus of treatment must be to reduce stroke risk through anticoagulation. Stroke risk can be assessed through use of the CHAD2DS2-VASc tool and anticoagulant treatment is likely to be unnecessary only in males with a score of 0 and females with a score of 1. Bleeding risk should be evaluated using HAS-BLED or ORBIT scores to identify any potentially reducible risks such as high blood pressure or medications.6
REVIEW
Recommended review periods will depend on treatment strategies and individual patient needs but should be at least annually via structured recall. Routine review of individuals with AF should include:6
- Review of any symptoms and their control
- Stroke and bleeding risk
- Signs of bleeding/anaemia
- Renal function (if anticoagulated)
- Medication review including adherence
- Weight/BMI
- Review of CVD risk factors and any support required
- Review of overall health and wellbeing, including mental health
REFERENCES
1. British Heart Foundation. UK Factsheet. April 2023 https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf
2. Fuster V, Ryden L E, Asinger R W.et al American College of Cardiology/American Heart Association/European Society of Cardiology Board. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary Circulation 2001;104:2118–2150.
3. Lip GY, Lowe GD. ABC of atrial fibrillation. Antithrombotic treatment for atrial fibrillation. BMJ 1996;312:45.
4. Rienstra M, Lubitz SA, Mahida S, et al. Symptoms and functional status of patients with atrial fibrillation: state of the art and future research opportunities. Circulation 2012;125(23):2933-43.
5. Wasmer K, Eckardt L, Breithardt G. Predisposing factors for atrial fibrillation in the elderly. J Geriatr Cardiol 2017;14(3):179-184.
6. NICE NG196. Atrial Fibrillation: diagnosis and management; 2021 https://www.nice.org.uk/guidance/ng196