Practice Nurse bite-sized learning: Understanding Stable Angina
Joanne Haws RN MSc, Michaela Nuttall RGN MSc
Joanne Haws RN MSc, Clinical Director, Learn With Nurses
Michaela Nuttall RGN MSc, Founder & Director, Learn With Nurses
Angina is a pain or discomfort in the chest area that occurs when the heart muscle is not getting enough oxygen-containing blood to meet its needs.There are different types of angina but the most common type is stable angina, which usually happens during physical activity or emotional stress and lasts for a short period of time.1
WHAT’S THE PROBLEM?
The most common cause of angina is coronary artery disease (CHD), where the build-up of atheroma is reducing blood flow to the cardiac muscle cells. CHD is responsible for around 66,000 deaths in the UK each year, which amounts to one death every eight minutes. One in eight men will die from CHD and it kills more than twice as many women as breast cancer – most of these deaths a premature (before their 75th birthday) and are largely preventable.2
DIAGNOSIS
It is vital to distinguish intermittent stable symptoms from acute or recent chest pain or discomfort that could be caused by an acute coronary syndrome (ACS), which covers a range of conditions including unstable angina and myocardial infarction.Where ACS is suspected an emergency admission to hospital is required.3
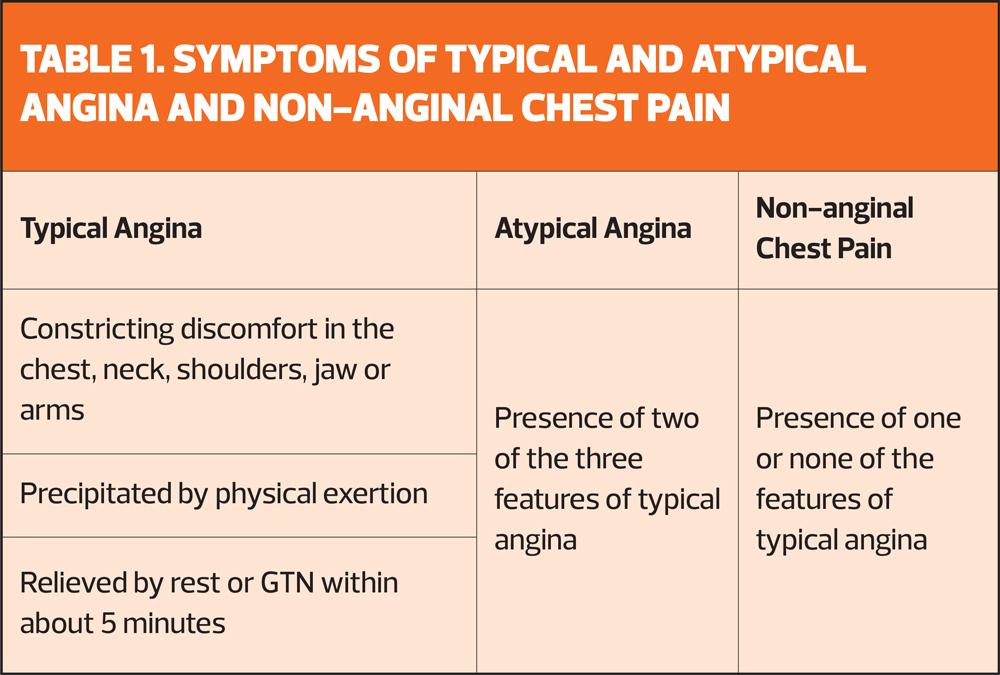
A diagnosis of stable angina will usually be made following a comprehensive clinical assessment including an evaluation of the symptoms (Table 1), cardiovascular risk factors and investigations including blood tests and a 12-lead ECG. This may be followed by further diagnostic testing including CT coronary angiography or an exercise ECG, and additional non-invasive functional testing or coronary angiography where indicated.3
MANAGEMENT
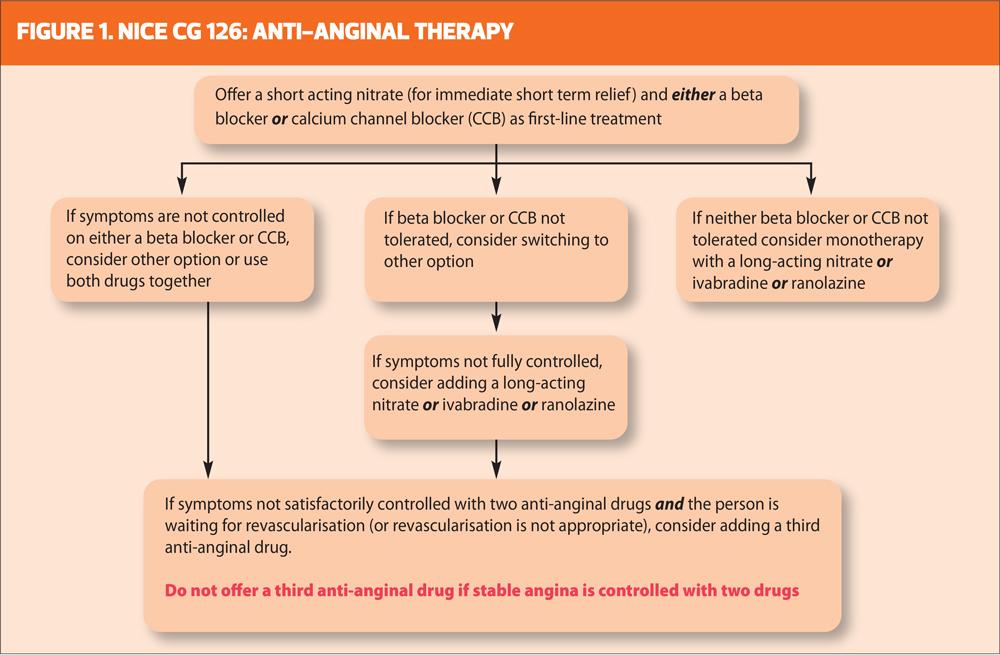
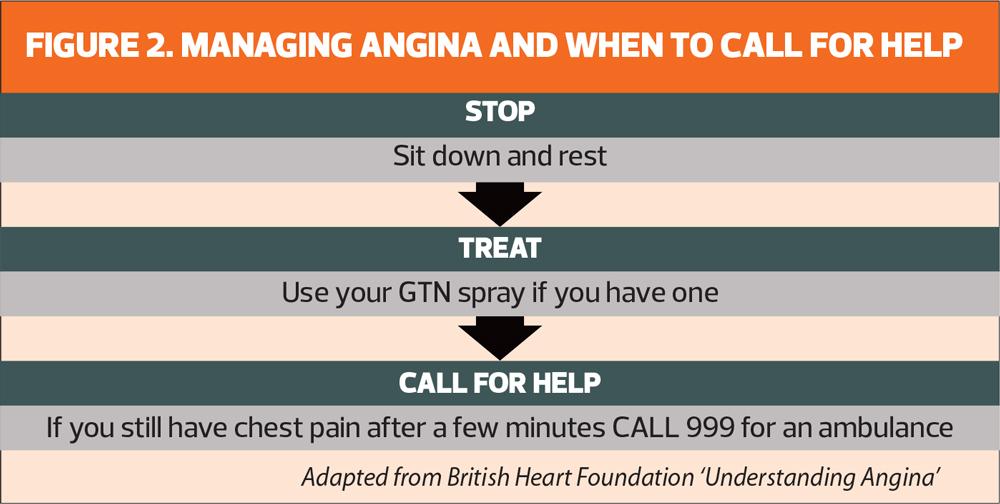
The common goals of angina management are to improve quality of life by reducing the number of angina episodes and the severity of symptoms, and to reduce the risk of acute cardiovascular events.It is essential that people with angina are aware of how to manage an episode and when to call for help (Figure 1).They should also be prescribed anti-anginal medication to reduce the number of episodes as well as secondary prevention therapies including an anti-platelet agent and lipid lowering medication (Figure 2).Revascularisation will usually only be considered where optimal medical therapy has failed to manage symptoms adequately.4
Management of risk factors through medication and lifestyle modification is a key strategy to delay the progress of CHD and reduce cardiovascular events. Patients will benefit from a programme of cardiac rehabilitation including home based programmes, where available. As well as practical information on risk reduction and managing episodes, such programmes will offer advice on coping and psychological support.
REVIEW OF SYMPTOMS
People with stable angina should be included in annual recall for review following a systematic approach including:
- Assessment of pulse rate and rhythm, blood pressure, weight and BMI
- Review renal function (including urinary albumin creatinine ratio), lipid levels, HbA1c
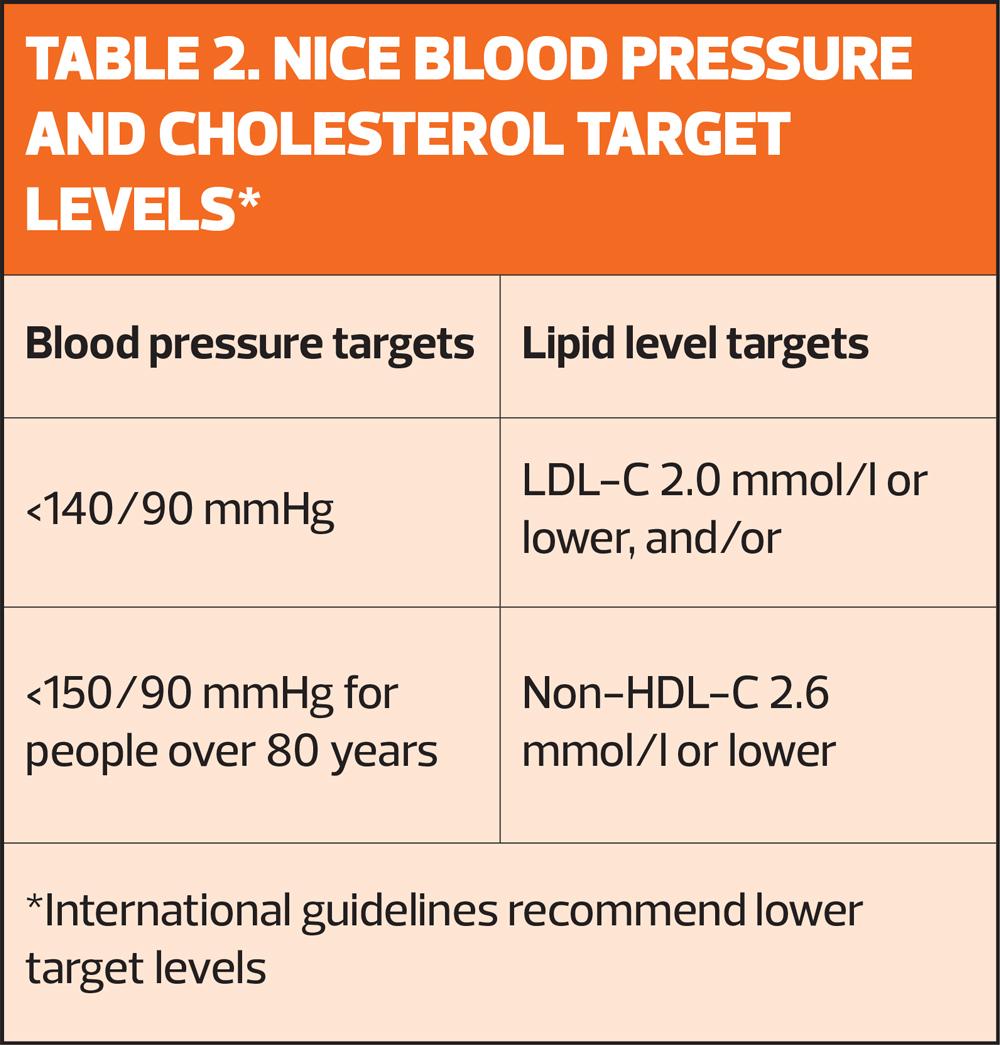
- Medication review including dosage, adherence and treatment targets (Table 2)
- Review functional status and ongoing rehabilitation needs
- Review of lifestyle factors and self-management strategies weight management, diet and nutrition, salt intake and physical activity
- Immunisations
- Review of overall health and wellbeing, including mental health
References
- American Heart Association. Stable Angina https://www.heart.org/en/health-topics/heart-attack/angina-chest-pain/angina-pectoris-stable-angina
- British Heart Foundation. UK CVD Statistics Fact Sheet.January 2025. https://www.bhf.org.uk/-/media/files/for-professionals/research/heart-statistics/bhf-cvd-statistics-uk-factsheet.pdf
- NICE CG95. Recent onset chest pain of suspected cardiac origin: assessment and diagnosis. Last updated November 2016 https://www.nice.org.uk/guidance/cg95/chapter/Recommendations#people-presenting-with-stable-chest-pain
- NICE CG126.Stable Angina: management. Last Updated August 2016 https://www.nice.org.uk/guidance/cg126/resources
Related articles
View all Articles