Practice Nurse Bite-Sized Learning: Hypertension
Joanne Haws
Joanne Haws
RN MSc
Clinical Director, Learn With Nurses
Michaela Nuttall
RGN MSc
Founder & Director, Learn With Nurses
Practice Nurse 2023;53(6):7-8
Almost a third of adults in the United Kingdom have persistently high blood pressure (hypertension) and it is one of the most important modifiable risk factors for cardiovascular disease
WHAT’S THE PROBLEM
Hypertension is the third biggest risk factor for premature deaths and disability, after smoking and poor diet, with at least half of all heart attacks and strokes being associated with high blood pressure.1 Hypertension places excess strain on the heart and kidneys, and within blood vessels where the endothelium can become damaged leading to a build-up of atheroma causing narrowing and leaving it susceptible to acute events.2
DETECTION
Most people with high blood pressure do not experience symptoms and will only be found through opportunistic case finding or other health consultations. Increasingly case finding takes place within communities and it is essential that pathways are in place to facilitate further monitoring and diagnosis in a clinical environment, such as general practice or participating community pharmacies. It is important that efforts are also made to reach population cohorts who are affected disproportionately by the burden of hypertension, such as those from Black African or Caribbean heritage who are less likely to get diagnosed and treated.3
DIAGNOSIS
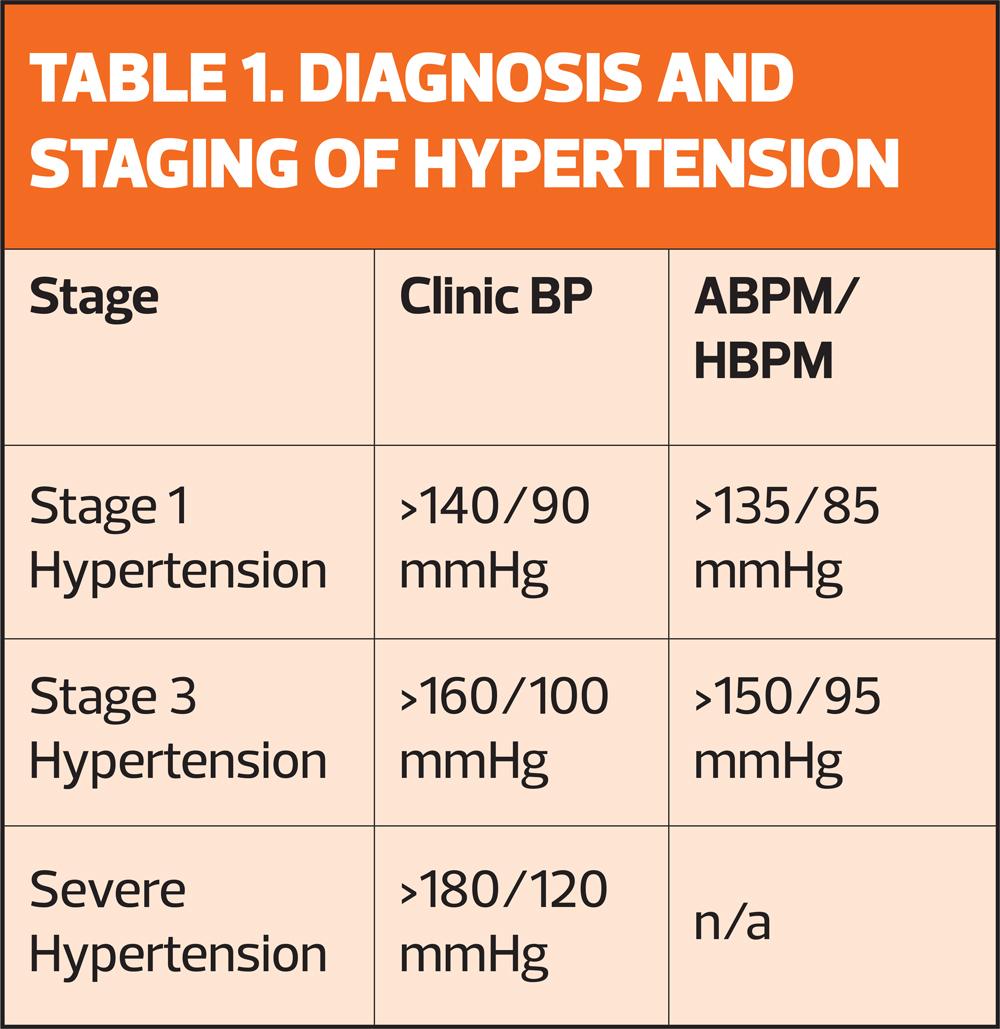
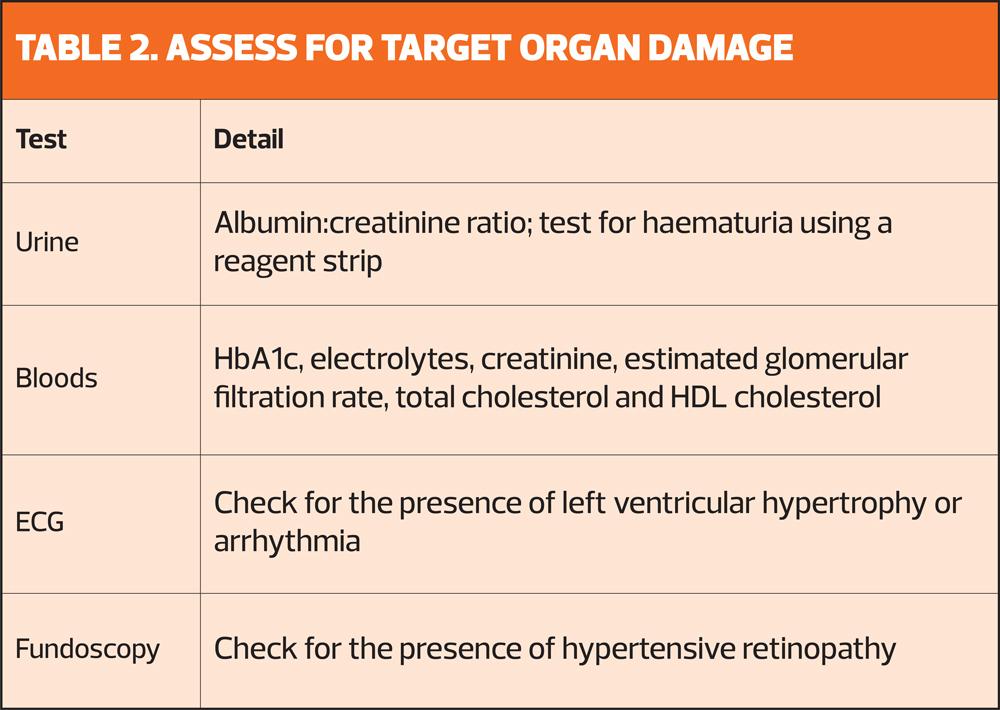
A single raised blood pressure (Clinic reading >140/90 mmHg) should always be followed up with Ambulatory Home Blood Pressure Monitoring (ABPM) or Home Blood Pressure Monitoring (HBPM).4 The average daytime reading is used to determine a diagnosis and stage the hypertension (Table 1). Once the diagnosis has been made the next step is to assess for organ damage (Table 2) and undertake a full cardiovascular risk assessment using QRisk or other recognised risk calculator.4
MANAGEMENT
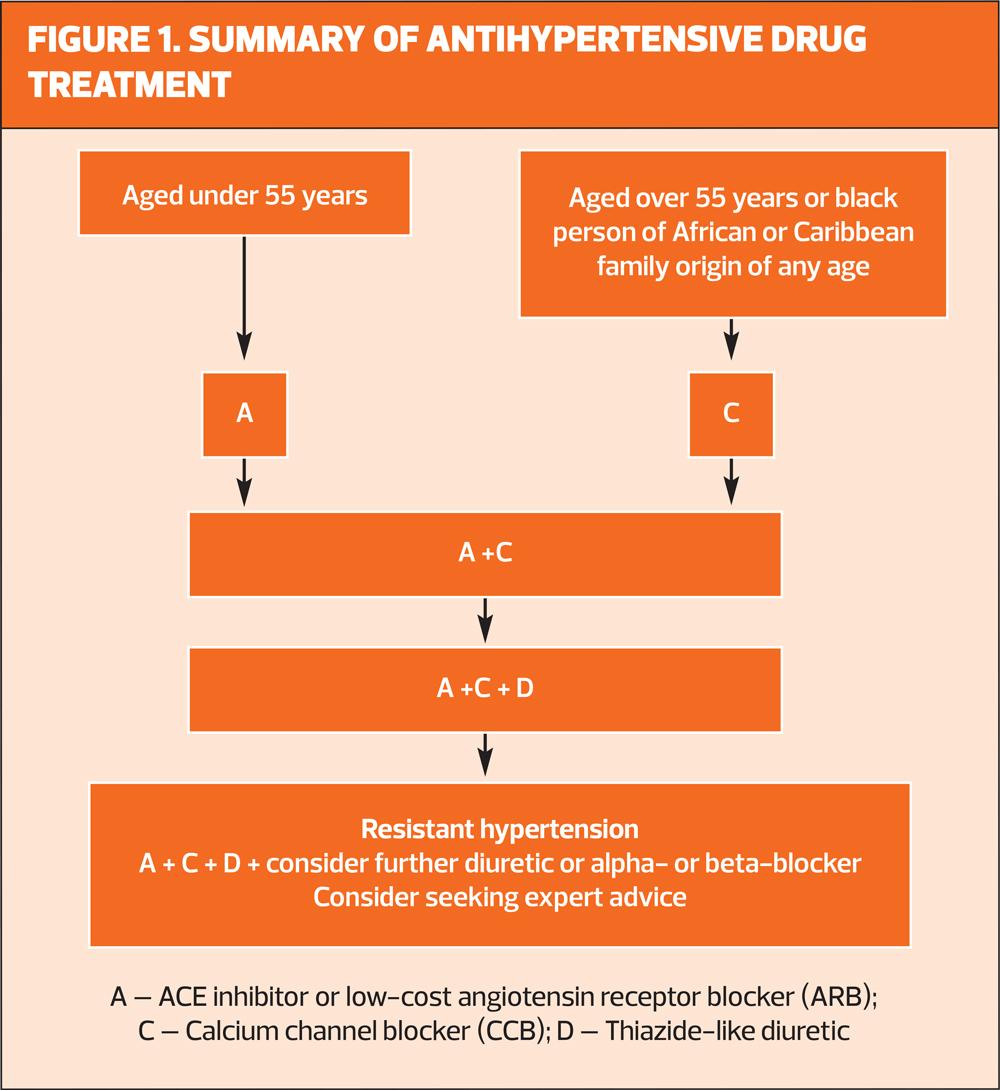
Anti-hypertensive medication may not be immediately indicated in people with stage one hypertension who have no target organ damage and a low 10-year CVD risk.4 Lifestyle modification can be very effective in lowering blood pressure if achieved and maintained. Where medication is indicated, NICE recommends starting the patient on first line monotherapy and adding in other therapies as required until the target blood pressure is reached (Figure 1).4 Most patients will require combination therapy to achieve optimal blood pressure lowering and improve long term outcomes.
REVIEW
- Check for any signs or symptoms of disease progression such as chest discomfort, shortness of breath or palpitations
- Check BP and/or review home readings
- Review renal function, lipid levels and HbA1c
- Review medication and adherence
- Weight/BMI
- Review CVD risk factors and any support required
- Review overall health and wellbeing, including mental health
REFERENCES
1. Public Health England. Health matters: combating high blood pressure; 2017. https://www.gov.uk/government/publications/health-matters-combating-high-blood-pressure/health-matters-combating-high-blood-pressure
2. Fuchs F, Whelton P. High Blood Pressure and Cardiovascular Disease. Hypertension 2020;75:285-292
3. Spence D, Rayner B. Hypertension in Blacks: Individualised Therapy Based on Renin/Aldosterone Phenotyping. Hypertension 2018;236-269
4. NICE NG136 Hypertension in adults: diagnosis and management; 2022. https://www.nice.org.uk/guidance/ng136