A new lipid pathway: its relevance for primary care
Rhiannon Edwards
Rhiannon Edwards
RGN, MSc
CVD Clinical Programme Lead. South West Academic Health Science Network
Practice Nurse 2022;52(1):14-18
Lipid lowering is a central strategy to reduce cardiovascular risk but elevated cholesterol remains under-diagnosed and under-treated. This guide aims to help the general practice nurse navigate the host of guidelines, national priorities, policies and service specifications and recently introduced drugs
Cardiovascular risk factors such as atrial fibrillation, raised blood pressure and elevated cholesterol are recognised in the NHS Long Term Plan (LTP) as under-diagnosed and under-treated.1 To support risk factor detection and management, work streams within primary care have been developed, and frameworks and pathways are being implemented nationally. These are evidence-based, and aim to provide clinicians with practical advice and guidance to enhance their understanding of screening opportunities and treatment decision aids.
This article will explore the resources available to primary care clinicians to facilitate patient-centred cholesterol management, the tools available to support clinical judgement, the opportunities that case finding in primary care clinical records can provide, using practice resources effectively, and treatment and management options. It will also consider the place of new medications, bempedoic acid and inclisiran, that have been recently introduced into the lipid pathway to reduce CVD risk and mortality.
OBJECTIVES
This article aims to:
- Explain the current national drivers – Vascular Checks programme, CVDPrevent, LTP and Cardiovascular Disease Diagnosis and Prevention Direct Enhanced Service (CVDDES) – to improve management of raised cholesterol
- Support the reader in making an informed decision on the case finding tools and resources that are available to improve detection and treatment of patients with raised cholesterol who are sub-optimally managed
- Highlight the updated NICE-endorsed Accelerated Access Collaborative lipid lowering pathway, to support the reader’s understanding of the options for lipid lowering medications
- Explain the mechanisms of action and uses of the newer lipid lowering medications, (bempedoic acid and inclisiran) and when they may be indicated, including any potential side effects and contraindications
NATIONAL DRIVERS OF CHANGE
The NHS England vascular health checks programme was rolled out in 2008,2 with the aim of improving prevention of cardiovascular disease (CVD). Developed as a systematic means of identifying those at a high risk of developing CVD, it encouraged lifestyle counselling and modifications alongside medical treatment, to prevent disease or reduce risk. These checks have demonstrated some success: 41% of eligible individuals accessed the checks3 and data demonstrate a significant reduction of CVD risk factors, including hypertension, cholesterol levels, smoking and central obesity.4
Prevention has remained a core direction in NHS England, with the NHS LTP allocating additional funding and resources to tackle prevention more holistically.1 It is hoped that this will not only help people stay healthy but also moderate demand on the NHS until 2025.
Direct Enhanced Service (DES) plans
The Network Contract CVDDES specification5 includes requirements for the delivery of a CVD prevention and diagnosis service by primary care networks, and aims to reduce the impact of the A, B, Cs of CVD (AF, high Blood pressure/hypertension and Cholesterol). As a measure to reduce workload during the pandemic, last year practices were asked to focus on hypertension. From April 2022, the objectives will be expanded to include detection and management of AF, and addressing cholesterol in the context of CVD risk, including the detection and management of FH. Nonetheless, the recent surge in cases of the omicron variant of COVID-19 could impact these objectives.
CVDPrevent audit
The CVDPrevent audit Quality Improvement has been developed to support the CVDDES. It provides real-time practice level data on diagnosis and treatment of the high-risk conditions for CVD.6 The CVDPrevent audit is a resource available to primary care to identify ‘at risk’ individuals, focus on the gaps that exist in current service delivery, and consider opportunities to redesign pathways of care to address barriers. This could include utilising the workforce differently, and building capacity in the system by pooling resources and upskilling staff to manage elements of patient care. As suggested by the Primary Care Workforce Commission,7 in terms of the significant challenges in primary care, this is an essential component to consider with an ageing population, increased workload and increasingly complex conditions. Healthcare professionals will need to develop new roles, and patients will begin to be seen by new types of healthcare professional.
Case-finding tools to support lipid management and FH
Case finding tools in general practice patient administration systems have long been in existence, linked with auditing and managing the care of patients with long term conditions and to demonstrate achievement of Quality Outcomes Framework (QOF) indicators. There have been many tools focusing on prevention developed locally and used nationally, but two main systems that focus on the lipid pathway are available in primary care. These are produced by the Clinical Digital Resource Collaborative (CDRC) and the University College London Partnership (UCLP).
The CDRC tool has been developed alongside clinicians in the North East of England and can work with both EMIS and SystmOne software. Aspects of this tool include resources to help practices manage their patients’ lipids, and search options for observing the current status of lipid management at practice, PCNs and CCG level, enabling benchmarking within regions. One of the other useful aspects of this tool is the ability to view previous and current medication, to support conversations with patients about their treatment history, and offer opportunities to trial alternative lipid lowering medication. This can be done alongside the statin intolerance pathway (awaiting an update in line with the recently published Lipid pathway), created by the Accelerated Access Collaborative and available at https://www.england.nhs.uk/aac/wp-content/uploads/sites/50/2020/08/Statin-Intolerance-Pathway-NEW.pdf. In addition, CDCR has opportunities to identify those who may meet FH criteria and those eligible for proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors. More information can be found in Lipids, Familial Hypercholesterolaemia (FH) and PCSK9i Guide for SystmOne at https://cdrc.nhs.uk/resources/fh/lipids-familial-hypercholesterolaemia-fh-and-pcsk9i-systmone-guide/
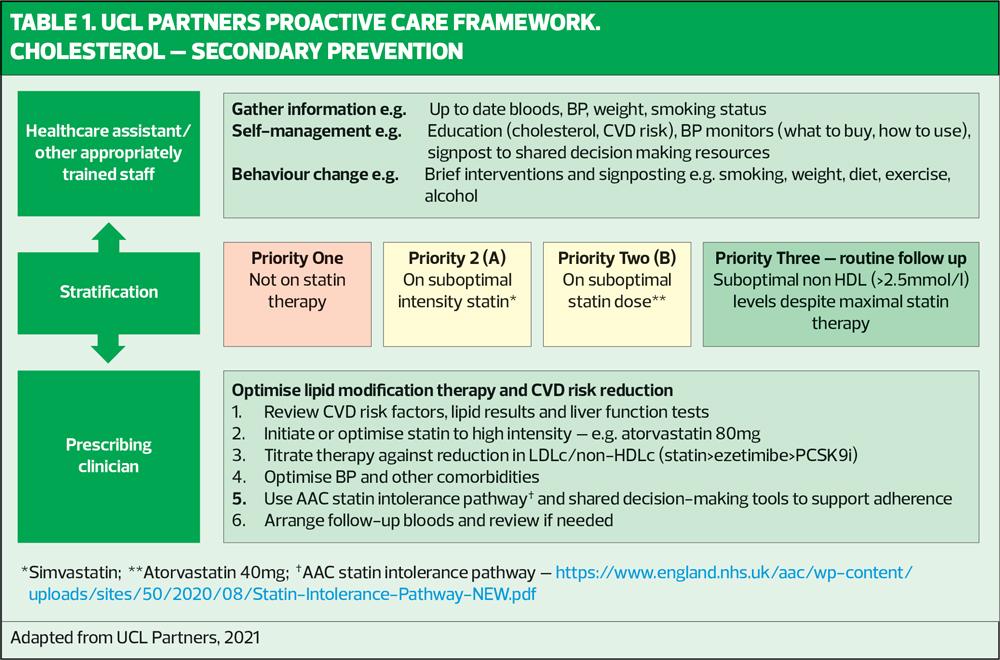
The UCLP has also developed and defined a search and stratification tool alongside their Proactive Care Framework. This tool can be adapted to meet local needs if required, and it supports decision-making by stratifying patients into low, medium, and high-risk of deterioration. As a package of support from primary care, the case finding tools not only highlight patients in need of review, but they also offer signposting to relevant NICE and other clinical guidance. The educational resources collated within the package enable clinicians to provide relevant information to patients to promote understanding of the impact of treatment and therefore support concordance with prescribed medication.
Decision-making support
Since the start of the COVID-19 pandemic, there has been a lack of chronic condition management across all sectors due to the risks associated with the virus and limited NHS capacity. This could jeopardise the sustainability of healthcare systems by worsening the condition of patients with chronic conditions.8 Supporting the heath service to maintain some level of chronic disease management in primary care during COVID-19 recovery was the rationale behind the development of the UCLP Proactive Care Frameworks (https://uclpartners.com/proactive-care/ ).
The Frameworks were developed to support stratification of higher risk patients, so that all members of the primary care team could prioritise patient care, and more effectively manage workload pressures; they aim to maximise remote care and optimise personalisation and support for self-care.9 Supported by the UCLP case finding search tool, clinicians are able to search for patients at the greatest risk, and categorise them into priority groups. These individuals can then be managed using appropriate clinician support (Table 1).
TREATMENT PATHWAYS
Healthcare pathways have been used routinely for the past four decades to reduce unwarranted variation and improve patient outcomes.10
Pathways are not rules to be followed, but are instead guidelines for the optimal sequencing and timing of interventions by clinicians, nurses and other healthcare professionals, for a particular diagnosis or procedure, designed to minimise delays and resource utilisation and to maximise the quality of care.11
The National Institute of Health and Care Excellence (NICE) uses evidence to construct guidelines, quality standards, pathways and technology appraisals, so clinicians and commissioners can ensure both the NHS and patients have access to robust decision-making resources. Included in the NICE portfolio are resources for lipid modification, hyperlipidaemia (including FH), PCSK9 inhibitors (alirocumab and evolocumab) and inclisiran. NICE pathways also offer robust patient decision-making aids. With the increasing recognition that patients should be involved in decision-making with regard to their treatment plan,12 this is key to enhancing patient concordance with treatment.
In addition, the NHS Accelerated Access Collaborative provides mechanisms to support faster adoption of innovations into the NHS. In June 2020, their first lipid pathway was produced and endorsed by NICE, alongside additional documents including the statin intolerance pathway. These resources gave clinicians the first opportunity to see all the relevant information on one page.
LIPID LOWERING PATHWAY
The NICE clinical pathway for lipid modification includes interactive flow charts to support clinical decision-making, as well as signposting to additional documents such as quality standards.
(NB. NICE has announced that the Pathways site will not be supported from Spring 2022 and subsequently may not reflect latest guidance)
Although the pathways can aid understanding of the topic area and provides access to further information, they can be challenging to use during brief consultations. Therefore, the AAC has created a NICE-endorsed lipid ‘pathway on a page’ which collates all of the NICE guidance from primary to secondary prevention in one easy-to-view document. This was updated in December 2021 and is available at https://www.england.nhs.uk/aac/wp-content/uploads/sites/50/2020/04/Lipid-Management-Pathway-NEW-version-4.pdf
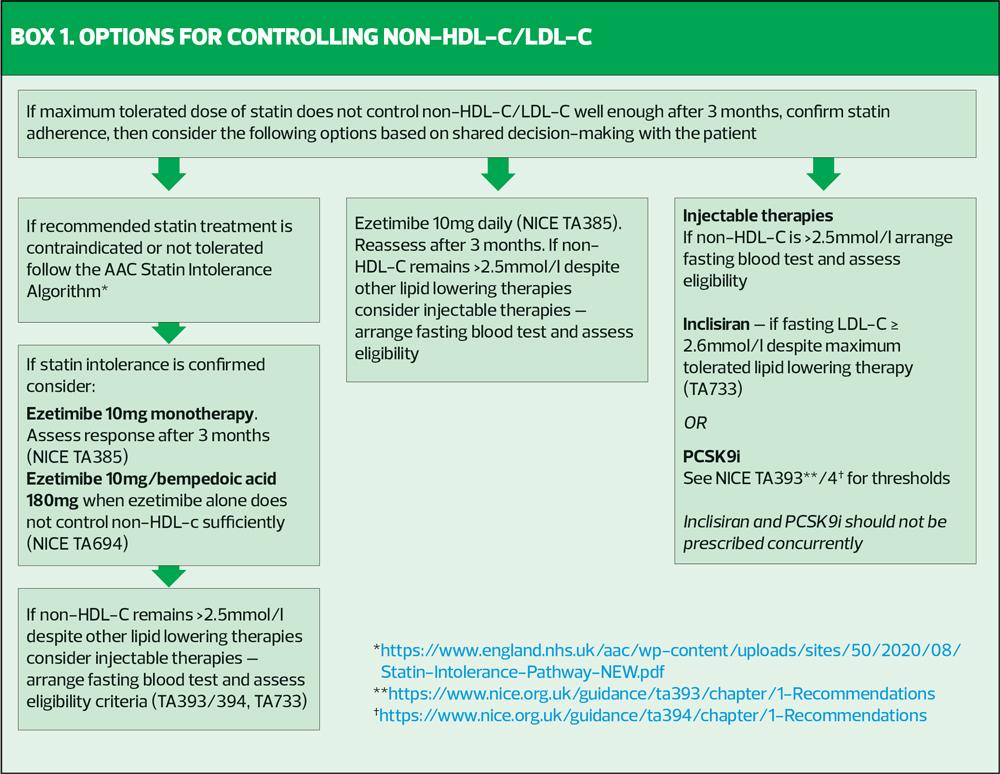
The AAC pathway sets out criteria for prescribing statins, plus or minus additional lipid lowering drugs, and also gives a clear indication for when newer, injectable therapies should be considered (Box 1). As general practice nurses will already be familiar with the use of statins and ezetimibe, and PCSK9i is initiated in specialist settings, their place in therapy will not be rehearsed here. However, new medications have been included in this pathway, so a brief explanation of bempedoic acid and inclisiran can be found below, to improve the understanding of the reader regarding the opportunity to reduce low density lipoprotein cholesterol (LDL-C) levels further, with the focus of ensuring the patients cholesterol is managed to target.
It should be noted that neither of these drugs have CVD mortality outcome data, although robust evidence exists for causal links on LDL-C lowering and a reduction in atherosclerotic CVD.13,14 NICE guidance recommends that where possible, these drugs should always be initiated after statins, unless statins are not tolerated.
Bempedoic acid
Bempedoic acid is an oral medication and has a similar mode of action to statin therapy in terms of its impact on the suppression of cholesterol ‘synthesis’, compensatory LDLR upregulation, and LDL particle clearance from the blood. Bempedoic acid works higher up the same pathway as statins by inhibiting the ATP-citrate lyase (ACL) enzyme rather than 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA) reductase. Bempedoic acid is a prodrug and can therefore only be activated by the enzyme ACSVL1, which is only present in liver cells, not skeletal muscle.15 This means that bempedoic acid does not impact on skeletal muscle, and potentially avoids the myotoxicity (e.g. rhabdomyolysis) associated with statin therapy.16 As previously mentioned, there is currently no specific evidence of a reduction in major cardiovascular events, however the CLEAR outcomes trial will enable further understanding of the mechanisms of action and will report in the second half of 2022.17 The AAC considers bempedoic acid suitable for primary care prescribing alongside maximum tolerated statins and other lipid lowering medications. It is indicated in both primary and secondary prevention of CVD, where LDL-C levels have not been reduced to target or where statins are contraindicated or intolerance has been confirmed.18
Adverse effects: Common or very common: anaemia, gout, hyperuricaemia (discontinue treatment when experienced alongside gout) and pain in extremity. Unknown frequency: diarrhoea, muscle spasms and nausea.19
Discontinue treatment if transaminase levels persist at 3 x upper limit of normal.
Contraindications and cautions: avoid in pregnancy and breastfeeding
Inclisiran
Proprotein convertase subtilisin-kexin type 9 (PCSK9) is an enzyme that became relevant in the understanding of cholesterol metabolism in 2003.20 Identified as a gain of function genetic mutation during screening for FH, it showed a significant phenotype (physical representation) of the condition. The PCSK9 enzyme is produced in the liver and is responsible for LDL receptor degradation. This degradation reduces the number of LDL receptors and therefore increases circulating LDL cholesterol. Consequently, PCSK9 was considered a highly promising target for LDL-C lowering and preventive therapies.21
PCSK9 inhibitors in the form of injectable monoclonal antibodies (alirocumab and evolocumab) have been used in routine secondary care practice since 2009 and have shown reductions of 60-80% in LDL-C in those with hypercholesterolaemia, in addition to maximum tolerated statin therapy.22
Inclisiran is a novel therapy targeting the ribonucleic acid (RNA) (a molecule that is essential in coding genes) responsible for creating the PCSK9 enzyme. The mechanism of action for this therapy is to use a synthetic small interfering RNA (siRNA), to bind and interfere with the PCSK9 messenger RNA (mRNA). This interference causes the mRNA to degrade and reduces the ability of protein coding to be completed, reducing levels of PCSK9.21,23 Due to its mechanism of action, regular dosing following initiation is only required six monthly, it is injected subcutaneously and can be administered in general practice. In studies, this treatment demonstrated a 50% reduction in LDL-C in those on maximum tolerated statin therapy. Inclisiran can be prescribed in primary care for those with atherosclerotic CVD, needing secondary prevention and with persistent LDL-C levels above 2.6mmol/l, who are on maximum tolerated statin therapy.24
Adverse effects: the only reported adverse reactions in patients treated with inclisiran were local reactions at the injection site (8.2%).25 However, this is a black triangle drug, and therefore all potential side effects should be reported through the yellow card scheme.
Contraindications and cautions: The only contraindication listed in the summary of product characteristics is hypersensitivity to the excipients (sodium hydroxide and phosphoric acid). Inclisiran is eliminated renally, therefore haemodialysis should not be performed for 72 hours after administration; no dose adjustments are necessary for patients with renal impairment, but inclisiran should be used with caution in patients with severe renal impairment and in patients with severe hepatic impairment. There are no data for the use of inclisiran in pregnancy or breastfeeding.25
CONCLUSION
This article is intended to take the reader through a practical guide to the lipid pathway and the resources available to primary care to support management of a patient’s cholesterol levels. The updated pathway incorporates new and novel treatment options for patients to support them in understanding the need for concordance with treatment and reduce their risk of developing CVD. There are many challenges and complexities that exist in the management of hypercholesterolaemia. The tools and resources suggested here aim to support healthcare professionals to strategically prioritise those at risk, and communicate relevant information to patients to ensure they are involved in their care.
REFERENCES
1. NHS England. The NHS Long Term Plan; 2019. https://www.longtermplan.nhs.uk
2. Department of Health. Putting prevention first. Vascular checks: risk assessment and management; 2008. http://data.parliament.uk/DepositedPapers/Files/DEP2008-0910/DEP2008-0910.pdf (archived)
3. Office for Health Improvement & Disparities (OHID); December 2021. Preventing illness and improving health for all: a review of the NHS health check programme and recommendations. https://www.gov.uk/government/publications/nhs-health-check-programme-review/preventing-illness-and-improving-health-for-all-a-review-of-the-nhs-health-check-programme-and-recommendations
4. Cochrane T, Davey R, Iqbal Z, et al. NHS health checks through general practice: randomised trial of population cardiovascular risk reduction. BMC Public Health 2012;12:944
5. NHS England (2021) Cardiovascular disease prevention and diagnosis: supplementary guidance. https://www.england.nhs.uk/wp-content/uploads/2021/09/B0951-v-network-contract-des-20-21-cvd-supplementary-guidance.pdf
6. NHS Digital. Cardiovascular Disease Prevention Audit (CVDPREVENT). https://digital.nhs.uk/services/general-practice-gp-collections/service-information/cardiovascular-disease-prevention-audit-cvdprevent
7. Primary Care Workforce Commission. The future of primary care: Creating teams for tomorrow; 2015. https://napc.co.uk/wp-content/uploads/2017/09/Future_of_primary_care.pdf
8. Palmer K, Monaco A, Kivipelto M et al (2020)The potential long term impact of the COVID 19 outbreak on patients with non communicable diseases in Europe: consequences for healthy ageing Aging Clinical and Experimental Research 2020;32:1189–1194 https://link.springer.com/content/pdf/10.1007/s40520-020-01601-4.pdf
9. Kearney M, Shah D, Peate S, et al. The UCL Partners Proactive Care Frameworks – Optimising CVD Prevention post Covid. Innovation to restore and improve care in the High-risk conditions and prevent heart attacks and strokes at scale. Heart 2021;107(Suppl 1):A1–A185.
10. Vanhaecht K, Panella M, van Zelm R, et al. An overview on the history and concept of care pathways as complex interventions. International Journal of Care Pathways 2010;14:117–123.
11. Cheah T S (1998) Clinical Pathways - The New Paradigm in Healthcare? Med J Malaysia 1998;53(1): 87–96
12. Spatz E, Krumholz H, Moulton B. The new era of informed consent getting to a reasonable-patient standard through shared decision making. JAMA 2016;315(19):2063–4
13. Rached F, Santos R (2020) The role of statins in current guidelines. Current Atherosclerosis Reports 2020;22(50):1–11.
14. Chen Z, Peto R, Collins R, et al. Serum cholesterol concentration and coronary heart disease in population with low cholesterol concentrations. BMJ 1991;303(6797):276–82.
15. Ray K, Phil M, Bays H, et al. Safety and Efficacy of Bempedoic Acid to Reduce LDL Cholesterol. N Engl J Med 2019;380:1022–32
16. Pinkosky S, Newton R , Day E, et al Liver-specific ATP-citrate lyase inhibition by bempedoic acid decreases LDL-C and attenuates atherosclerosis. Nature Communications 2016;7(13457):1–13.
17. Nicholls S, Lincoff M, Bays H, et al. Rationale and design of the CLEAR-outcomes trial: Evaluating the effect of bempedoic acid on cardiovascular events in patients with statin intolerance Am Heart J 2021;235:104-12
18. NICE TA694. Bempedoic acid with ezetimibe for treating primary hypercholesterolaemia or mixed dyslipidaemia; 2021. https://www.nice.org.uk/guidance/ta694
19. Abifadel M, Varret M, Rabes JP, et al. Mutations in PCSK9 cause autosomal dominant hypercholesterolemia. Nat Genet. 2003;34(2):154–6
20. Sinning D, Landmesser U. Low-density lipoprotein-cholesterol lowering strategies for prevention of atherosclerotic cardiovascular disease: Focus on siRNA treatment targeting PCSK9 (Inclisiran) Current Cardiology Reports 2020;22:176
21. Stein EA, Mellis S, Yancopoulos GD, et al. 2012. Effect of a monoclonal antibody to PCSK9 on LDL cholesterol. N Engl J Med 2012;366:1108–18
22. Ray K. Wright R S, Kallend D, et al for the ORION-10 and ORION-11 Investigators. Two phase 3 trials of inclisiran in patients with elevated LDL cholesterol. N Engl J Med 2020; 382:1507-1519
23. NICE TA733. Inclisiran for treating primary hypercholesterolaemia or mixed dyslipidaemia Technology appraisal guidance; 2021. https://www.nice.org.uk/guidance/ta733
24. Nilendo (bempedoic acid) 180mg film-coated tablets. Summary of Product Characteristics; 2020. https://www.medicines.org.uk/emc/product/11743/smpc#gref
25. Leqvio (inclisiran) 284mg solution for injection in pre filled syringe. Summary of Product Characteristics; 2021. https://www.medicines.org.uk/emc/product/12039/smpc#gref