MART initiation for beginners
Nikki Lopez, MSc, RGN, Respiratory Nurse Specialist and Nurse Manager, South Coast Medical Group PCN Dorset Member, PCRS Education Committee NHS England Respiratory Champion
Practice Nurse 2025;55(5):22-25
A nurse-led service improvement project (SIP) designed to enhance confidence and knowledge in initiating Maintenance and Reliever Therapy (MART) for patients with uncontrolled asthma has demonstrated significant improvements in prescribing behaviour
INTRODUCTION
Maintenance and Reliever Therapy (MART) with inhaled corticosteroid (ICS)–formoterol has emerged as a cornerstone of contemporary asthma management. Evidence from randomised controlled trials,1,2 large observational studies,3 and national and international guidelines,4,5 consistently demonstrates that MART reduces severe exacerbations, lowers cumulative steroid exposure, and improves safety compared with short-acting beta-agonist (SABA)-based regimens.
Despite this, uptake of MART across UK primary care remains inconsistent. Barriers include prescribing inertia, clinician uncertainty, patient attachment to SABA inhalers, and fragmented service pathways. Within South Coast Medical Group (SCMG), a Primary Care Network (PCN) in Dorset, local audits identified high SABA prescribing and low clinician confidence in MART initiation. In response, a service improvement project was implemented, combining multidisciplinary training, deprescribing policies, FeNO diagnostics, digital patient support, and coding templates. Early outcomes showed >90 MART initiations, a 4% reduction in SABA prescribing (double the local average), and a 22% increase in review coverage for high-risk cohorts.
BACKGROUND
Asthma remains a leading cause of morbidity in the United Kingdom, with 5.4 million people currently receiving treatment.6 Despite advances in therapeutics, the UK continues to record disproportionately high asthma mortality compared to other European nations.7 The National Review of Asthma Deaths (NRAD) highlighted that two-thirds of deaths involved avoidable factors such as SABA overuse and underuse of ICS,7 while the National Child Mortality Database confirmed ongoing inequalities, with children from deprived communities more likely to die from asthma.8
In response, guidelines from BTS/NICE/SIGN, and GINA now strongly discourage SABA-only treatment and advocate for ICS-containing regimens, including MART.4,5MART enables patients to use a single ICS–formoterol inhaler for both daily maintenance and symptom relief, offering dual benefits of bronchodilation and anti-inflammatory action. Clinical evidence demonstrates reductions in exacerbations and steroid exposure, making MART a transformative approach for many patients.
Yet despite strong evidence, adoption in UK primary care is inconsistent. Entrenched prescribing patterns, clinician uncertainty, and patient attachment to the ‘blue inhaler’ act as barriers.9 Nurses, who often lead asthma reviews and inhaler education, are uniquely placed to address these challenges and support safe implementation.10
CLINICAL RATIONALE
Traditional asthma management centred on the use of SABAs for immediate symptom relief, with ICS prescribed separately as a preventer. While SABAs provide rapid bronchodilation and are perceived by patients as effective in the moment, reliance on them as monotherapy has been strongly associated with increased risk of exacerbations, hospitalisations, and mortality.3 This over-reliance has been particularly problematic in the UK, where audits repeatedly show high SABA prescribing, despite clear guidance to the contrary.6,7
MART addresses these risks by ensuring that every reliever dose is coupled with a dose of ICS, directly targeting airway inflammation alongside bronchoconstriction: patients are no longer exposed to ‘naked bronchodilation’ but instead receive anti-inflammatory treatment proportionate to their symptom burden.5 By aligning reliever use with inflammation control, MART tackles one of the most dangerous aspects of asthma care – the disconnect between symptom relief and disease modification.
From a pharmacological perspective, formoterol is uniquely suited to this dual role. Unlike other long-acting beta-agonists (LABAs), formoterol has a rapid onset of action, with bronchodilation evident within minutes, comparable to salbutamol.11 Yet it also provides prolonged action for up to 12 hours, reducing the risk of symptom recurrence. When combined with budesonide or beclomethasone, this creates an inhaler that provides both immediate relief and sustained anti-inflammatory activity. For patients, this dual mechanism means that symptom-driven reliever use automatically escalates ICS exposure at times of increased airway inflammation, thereby reducing exacerbation risk.
For nurses, this pharmacological advantage translates into practical clinical benefits. MART simplifies treatment regimens by consolidating preventer and reliever into a single device. This reduces the cognitive and behavioural burden on patients, many of whom struggle with adherence to multiple inhalers.10 Fewer devices also create more consistent opportunities for nurses to teach and reinforce inhaler technique, an area where up to 80% of patients demonstrate errors.12 By embedding ICS into every reliever dose, MART also reduces the reliance on adherence to scheduled preventer therapy, a common challenge in younger populations and in deprived communities where health literacy and engagement may be lower.8
Critically, however, this simplification is not without risks. Patients must be educated about maximum daily doses to prevent inadvertent overuse of formoterol, which may result in tachycardia, tremor, or hypokalaemia if misused.5 Conversely, some patients may underuse their MART inhaler due to ‘steroid anxiety,’ believing that each additional puff delivers excessive corticosteroid exposure. Nurses therefore play a central role in addressing misconceptions, contextualising the evidence that MART often results in lower overall ICS exposure compared with traditional maintenance regimens,1 while simultaneously reinforcing dose limits.
Patient behaviour is typically shaped by capability, opportunity, and motivation.13 SABAs score highly on all three dimensions: they are simple to use (capability), often on repeat prescription (opportunity), and provide immediate relief (motivation). ICS, by contrast, provides no immediate symptomatic reinforcement, undermining motivation. MART rebalances these drivers by embedding anti-inflammatory therapy into a behaviour patients are already motivated to perform – taking their reliever when symptomatic.
Equity considerations further strengthen the rationale. Data from the NCMD highlight that asthma mortality disproportionately affects children in deprived communities. These groups are also more likely to experience fragmented care and poor adherence.8 MART offers a pragmatic approach by reducing reliance on strict adherence to maintenance regimens and aligning treatment with real-world patterns of reliever use. While this does not replace the need for broader action on social determinants of health (e.g. housing quality, smoking prevalence, access to care), it offers a treatment strategy that may be more resilient to the realities of health inequality.
Finally, MART aligns with sustainability goals. By consolidating inhaler therapy, MART can reduce the overall number of devices prescribed. Combined with the option of using dry powder inhalers (DPIs), which have a lower carbon footprint than pressurised metered-dose inhalers,14 MART supports the NHS Net Zero agenda without compromising clinical outcomes.
In summary, the rationale for MART is multifaceted: it provides pharmacological superiority by combining rapid relief with anti-inflammatory action; behavioural alignment by embedding ICS into symptom-driven use; practical advantages through regimen simplification and reduced device burden; equity potential by reducing reliance on perfect adherence; and sustainability benefits through rationalised inhaler use. For practice nurses, MART offers a clinical tool that can directly improve safety while also serving as a platform for patient education, advocacy, and system-level leadership.
ARGUMENTS FOR AND AGAINST MART
Arguments in favour of MART
- Reduction in severe exacerbations
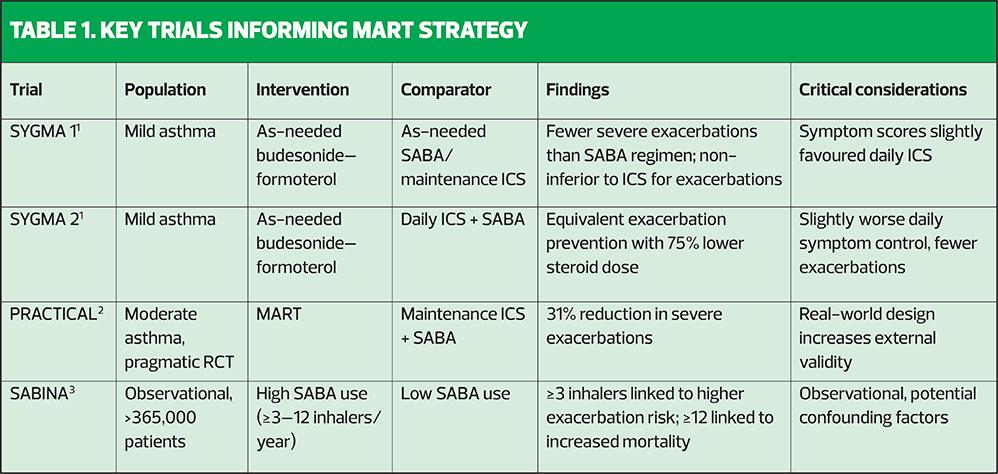
The strongest argument in favour of MART is the consistent reduction in severe exacerbations across multiple randomised controlled trials and systematic reviews (See Table 1). In the SYGMA studies, budesonide–formoterol as reliever therapy significantly reduced the rate of severe exacerbations compared with SABA-only treatment.1 Similarly, the pragmatic PRACTICAL trial demonstrated a 31% reduction in severe exacerbations for MART compared to traditional ICS plus SABA regimens.2 Systematic reviews have confirmed that these results are robust across diverse populations and healthcare settings.11 From a nursing perspective, the prevention of exacerbations is not only clinically important but also central to reducing avoidable hospital admissions, improving patient quality of life, and addressing the workload pressures that result from frequent unscheduled asthma care. - Lower cumulative corticosteroid exposure
Another compelling rationale is that MART allows effective control with substantially lower cumulative ICS exposure. SYGMA 2, for example, demonstrated equivalent exacerbation prevention with 75% less steroid exposure compared with daily maintenance ICS plus SABA.1 Given that long-term ICS exposure is associated with systemic side effects such as adrenal suppression, osteoporosis, and cataracts,15 this reduction represents a significant safety benefit. Practice nurses are often at the forefront of monitoring these long-term complications, making this outcome particularly relevant to their clinical leadership role. - Simplified regimens and improved adherence
MART consolidates preventer and reliever into a single inhaler, reducing treatment complexity. Adherence to asthma therapy is notoriously poor, with studies showing up to 50% of patients fail to take ICS as prescribed.10 By linking ICS to symptom-driven use, MART helps overcome this challenge. Patients are more likely to take treatment when symptomatic, meaning MART ensures that reliever use simultaneously escalates ICS dosing in periods of increased risk. For practice nurses, this simplification makes education and inhaler technique monitoring more straightforward, as fewer devices need to be demonstrated, checked, and prescribed. - Guideline convergence and policy support
Historically, variations in guideline recommendations created uncertainty among clinicians. However, recent harmonisation strengthens confidence. BTS/SIGN/NICE and GINA both now recommend MART and strongly advise against SABA-only treatment.4,5 This consensus reduces ambiguity and provides a clear mandate for practice change, aligning clinical practice with national safety and quality priorities. For practice nurses, this convergence legitimises advocacy for MART in multidisciplinary discussions and provides a foundation for leadership in local implementation.
Arguments against MART
- Symptom control nuances
While MART has proven efficacy in reducing exacerbations, daily symptom control scores are sometimes slightly less favourable compared with regular maintenance ICS. In SYGMA 1, patients on MART reported marginally worse symptom control and quality-of-life scores compared with those on regular ICS plus SABA.1 Although the difference was small, it highlights a trade-off: fewer severe exacerbations at the possible expense of slightly increased day-to-day symptoms. Nurses must be prepared to discuss this nuance in shared decision-making, ensuring that patients prioritise long-term safety without feeling that their daily comfort is disregarded.
2. Risk of misuse without adequate counselling
MART regimens are more complex in terms of dosing safety limits. Patients must understand maximum daily dose limits for budesonide–formoterol, as overuse risks tachycardia, tremor, and hypokalaemia.5 Conversely, some patients may underuse due to concerns about ‘steroid overexposure,’ particularly where misinformation about corticosteroids circulates. Inadequate counselling could therefore result in either insufficient anti-inflammatory treatment or harmful overuse. This places a significant educational burden on clinicians, particularly nurses, who must deliver clear, repeated, and tailored education.
3. Evidence gaps in vulnerable populations
The majority of MART trials focus on mild to moderate asthma in younger adult populations. Evidence for older adults, children under 12, and patients with multi-morbidity remains sparse.16 These groups may respond differently due to altered physiology, co-prescribing, or adherence challenges. Nurses providing holistic care to such populations must therefore exercise caution, tailoring treatment to individual needs and being alert to the limitations of generalising trial evidence.
4. Behavioural attachment to SABAs
Perhaps the most difficult barrier is behavioural rather than pharmacological. The ‘blue inhaler’ has become a cultural symbol of asthma control, representing immediate relief and safety.6 Patients often measure their disease control by how frequently they use their SABA, and some may perceive MART as less effective if they no longer experience the rapid ‘kick’ of salbutamol. Changing this deeply embedded behaviour requires sensitive, repeated education, motivational interviewing, and culturally appropriate communication strategies. Nurses, with their relational skills and longer patient contact time, are well placed to manage this transition but must recognise the depth of patient attachment to SABA.
CRITICAL BALANCE
The debate between MART and traditional regimens is therefore not one of absolutes but of trade-offs. While MART offers clear reductions in exacerbations and steroid exposure, it may compromise marginally on daily symptoms, requires careful patient education, and is supported by less evidence in vulnerable groups. Conversely, traditional ICS plus SABA regimens provide strong symptom control but carry higher risks of severe exacerbation and greater steroid exposure.
For practice nurses, the critical task is to navigate this balance in partnership with patients, ensuring that treatment choices are both evidence-based and personalised. This means moving beyond guideline adherence alone to embrace shared decision-making, patient advocacy, and ongoing evaluation of outcomes.
CASE STUDY: THE SCMG MART IMPLEMENTATION PROJECT
Problem Identification
SCMG audits revealed high SABA prescribing, with some patients receiving more than 12 inhalers annually, exceeding safety thresholds highlighted by SABINA.3 A local survey found 90% of GPs felt unconfident initiating MART, in contrast to confidence with SABA prescribing. This created a dual challenge of patient safety and workforce confidence.
Intervention Design
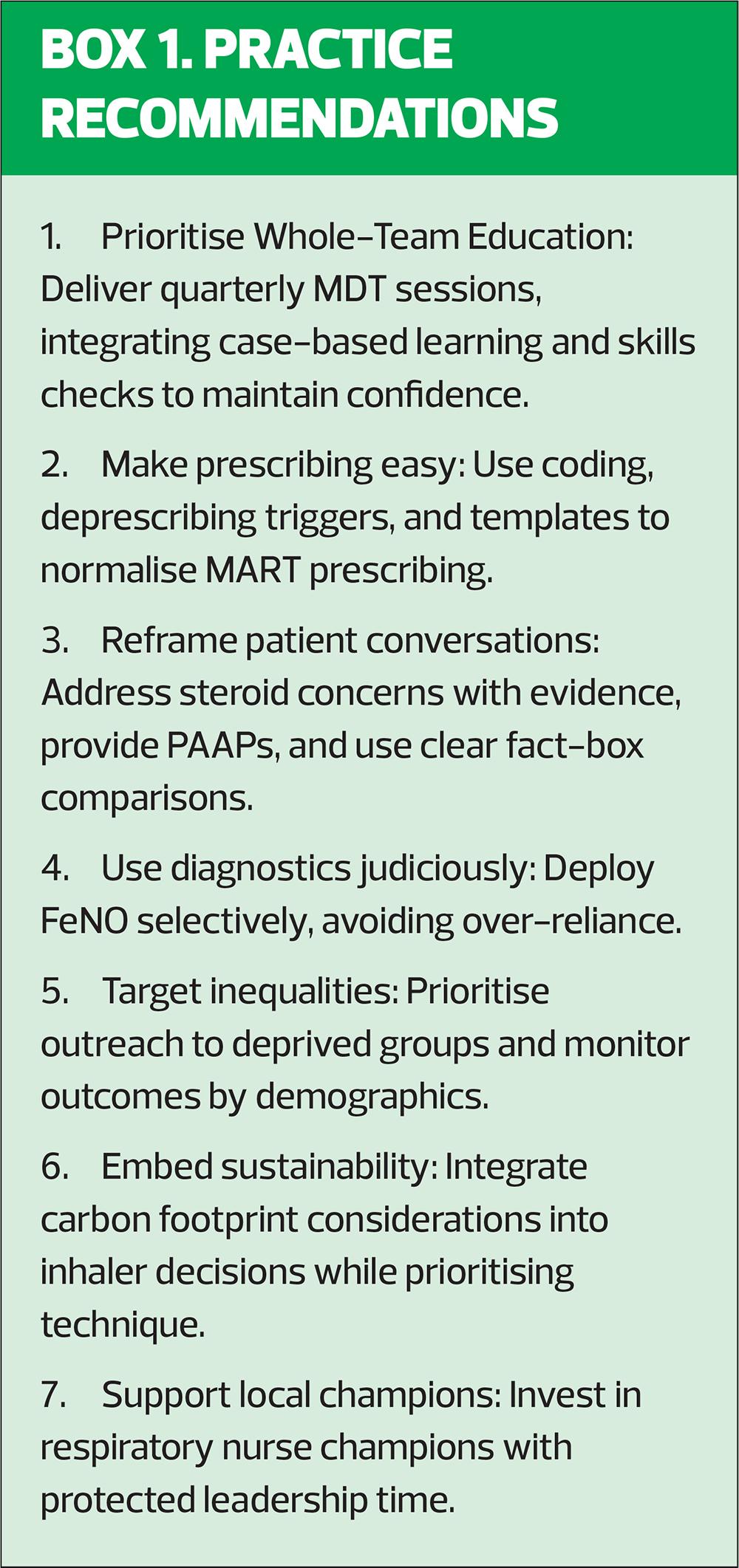
The project targeted capability, opportunity, and motivation. Components included:
- Education: MDT training, inhaler technique checks, PAAP development, case-based learning, and buddying with respiratory specialists.
- Deprescribing policy: Removal of inappropriate SABA repeats and ‘rescue’ steroids from repeat lists, creating review opportunities.
- Diagnostics: FeNO introduced at five sites, with contextual prompts in templates.
- Digital support: Symptom monitoring and education via Luscii app, with targeted outreach using Dorset Intelligence and Insight Service (DiiS).
- System redesign: Standardised SNOMED coding ([italics]XabRc[/]), prescribing templates with MART safeguards, and dashboards to track prescribing trends.
- Leadership: Respiratory nurse champions provided mentorship and modelled best practice.
- Sustainability: Inhaler choice considered both patient technique and carbon footprint.
Outcomes at 3 months
- 90 MART initiations.
- 4% reduction in SABA prescribing (vs 2% regional average).
- 22% increase in annual reviews among high-risk cohorts.
- Improved clinician confidence (>80% reporting readiness to initiate MART).
- Equity focus achieved outreach to patients in most deprived quintiles.
Critical reflections
Strengths included MDT engagement, system-level supports, and visible nurse leadership. Limitations included patient anxiety with deprescribing, potential miscoding, and limited digital engagement among older patients. Importantly, exacerbation rates and hospital admissions were not measured, limiting claims of clinical outcome improvement.
IMPLICATIONS FOR PRACTICE
The SCMG findings echo the wider evidence base: prescribing behaviour can be shifted through targeted education and system redesign. Early results align with international trial outcomes, but the absence of longer-term clinical endpoints limits conclusions.
The clinical and implementation evidence for MART with ICS–formoterol is increasingly difficult to ignore. Updated national and international guidance underscores the central message that SABA-only strategies are unsafe and that MART represents a safer, evidence-based alternative.4,5 Yet as the SCMG project illustrates, embedding MART into everyday practice is not straightforward. It requires more than a prescribing decision – it necessitates cultural, behavioural, and organisational change.
The case study demonstrates that with carefully structured interventions, meaningful change is achievable. Education sessions enhanced capability across the MDT; deprescribing policies created opportunities for review; digital and diagnostic tools provided clinical support; and visible nurse champions modelled new practice. These changes translated into measurable shifts in prescribing behaviour and workforce confidence within 3 months.
For practice nurses, the implications are profound. They are uniquely positioned to address misconceptions about corticosteroids, support patients through the behavioural transition away from the ‘blue inhaler,’ and ensure that MART regimens are safely embedded in personalised asthma action plans (PAAPs). Beyond clinical expertise, nurses also bring the relational skills needed to build trust, address equity gaps, and advocate for patient-centred decision-making.
Nevertheless, enthusiasm for MART must be balanced with critical caution. Evidence gaps remain for older adults, children, and those with complex multimorbidity. Symptom control nuances remind us that not every patient will experience improved daily symptoms on MART, even if exacerbation risk is reduced.1 These complexities reinforce the need for shared decision-making, where nurses act as facilitators of discussions that respect both evidence and individual patient preference.
MART implementation provides an opportunity to optimise inhaler prescribing in a way that is clinically effective and environmentally responsible, but patient technique and acceptability must always remain central.
Looking forward, the challenge is to sustain and scale such improvements. Local champions, as demonstrated in SCMG, play a vital role, but system-wide adoption will require investment in workforce development, digital infrastructure, and equity-focused outreach. Evaluations must extend beyond prescribing metrics to include clinical outcomes such as exacerbations, hospital admissions, and patient-reported quality of life, disaggregated by deprivation, ethnicity, and age to ensure that progress does not widen health inequalities.
Ultimately, MART adoption is about more than inhalers – it symbolises the ability of primary care teams to align with international best practice, to reduce avoidable harm, and to improve the safety and sustainability of asthma care. For practice nurses, the role extends beyond implementation to leadership: shaping policy, mentoring colleagues, and amplifying the patient voice.
If primary care embraces MART fully and thoughtfully, supported by nurse leadership, the potential gains are significant: fewer preventable deaths, reduced health inequalities, empowered patients, and more sustainable asthma care. The journey is challenging, but the direction is clear. Nurses are not just participants in this change – they are its catalysts and guardians.
CONCLUSION
Transitioning from SABA reliance to MART is not simply a pharmacological shift – it is a multifaceted cultural change. For practice nurses, this means leading education, supporting patients through behaviour change, and embedding equity and sustainability into everyday care. If implemented thoughtfully, MART offers the opportunity to reduce preventable morbidity and mortality, narrow inequalities, and align asthma management with the NHS Long Term Plan. Nurses are central to making this vision a reality.
References
- O’Byrne PM, FitzGerald JM, Bateman ED, et al. Inhaled combined budesonide–formoterol as needed in mild asthma. N Engl J Med 2018;378(20):1865–1876.
- Hardy J, Baggott C, Fingleton J, et al. Budesonide–formoterol reliever therapy versus maintenance budesonide plus terbutaline reliever therapy in adults with mild to moderate asthma (PRACTICAL): a 52-week, open-label, multicentre, superiority, randomised controlled trial. Lancet 2019;394(10202):919–928.
- Nwaru BI, Ekström M, Hasvold P, et al. Overuse of short-acting β2-agonists in asthma is associated with increased risk of exacerbation and mortality: a nationwide cohort study of the global SABINA programme. Eur Respir J 2020;55(4):1901872. doi:10.1183/13993003.01872-2019.
- NICE NG245. Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN); 2024. https://www.nice.org.uk/guidance/ng245
- Global Initiative for Asthma (GINA). GINA main report: global strategy for asthma management and prevention; 2024. https://ginasthma.org
- Asthma + Lung UK. Asthma facts and statistics; 2024. https://www.asthmaandlung.org.uk
- Royal College of Physicians. Why asthma still kills: the National Review of Asthma Deaths (NRAD); 2014. https://www.rcp.ac.uk/improving-care/resources/why-asthma-still-kills/
- National Child Mortality Database (NCMD) Child mortality and social deprivation; 2021. https://www.ncmd.info/publications/child-mortality-social-deprivation/
- Kuethe MC, Vaessen-Verberne AA, Elbers RG, Van Aalderen WM. Nurse versus physician-led asthma care for children. Cochrane Database Syst Rev 2013;2: CD009296.
- Dewey A. Cochrane Review Brief: Nurse Versus Physician-Led Care for the Management of Asthma. Online J Issues Nurs 2014;19(3). https://ojin.nursingworld.org/table-of-contents/volume-19-2014/number-3-september-2014/nurse-versus-physician-led-care-of-asthma/
- Beasley R, Pavord I, Papi A, et al. The role of ICS–formoterol reliever therapy in asthma management. J Allergy Clin Immunol Pract 2023;11(2):301–310.
- Price D, Bosnic-Anticevich S, Briggs A, et al. Inhaler competence in asthma: common errors, barriers to use and recommended solutions. Respir Med 2018;138:48–55.
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 2011;6(42): doi:10.1186/1748-5908-6-42.
- Janson C, Henderson R, Löfdahl M, et al. Carbon footprint impact of inhaler prescribing in the UK Thorax 2020;75(1): 82–84.
- Reddel HK, Bacharier LB, Bateman ED, et al. Global Initiative for Asthma Strategy 2017: executive summary and rationale for key changes. Am J Respir Crit Care Med 2017;195(5), pp. 557–582.
- Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. Lancet 2022;400(10359):476–490.
Related articles
View all Articles