FeNO testing in primary care – are we nearly there yet?
Carol Stonham MBE
Carol Stonham MBE
RN, MSc, Queen’s Nurse
NHS Gloucestershire CCG, Senior Nurse Practitioner – Respiratory
Executive Chair, PCRS
Practice Nurse 2021;51(05):18-21
FeNO testing is just one element of the diagnostic toolkit in respiratory care – but where does it fit in the patient pathway and what are its advantages and limitations?
As we think about how to restart respiratory services across the healthcare system the emphasis should not be on returning to how things were before the pandemic, but on ‘Building Back Better’.1 There is evidence from data collected by the National Asthma and COPD Audit Programme, for example, that prior to the disruption of respiratory services caused by the pandemic, there is room to improve the way more common respiratory diseases such as asthma and COPD were diagnosed in primary care.2
The use of spirometry, one of the most common respiratory diagnostic tests used for patients presenting with symptoms of breathlessness and cough, has stalled for over a year. This has resulted in a large, and mostly unknown, backlog of patients waiting for confirmation of a respiratory diagnosis.
The Primary Care Respiratory Society UK (PCRS) and the Association for Respiratory Technology and Physiology (ARTP) have issued joint guidance looking at the broad considerations necessary to restart diagnostic spirometry including risk assessment, patient stratification and potential models of delivery.3 However, to Build Back Better we need to look at the bigger picture. In this article we will consider if, how and where fractional exhaled nitric oxide (FeNO) testing would fit into a respiratory diagnostic patient pathway.
WHAT IS A FeNO TEST?
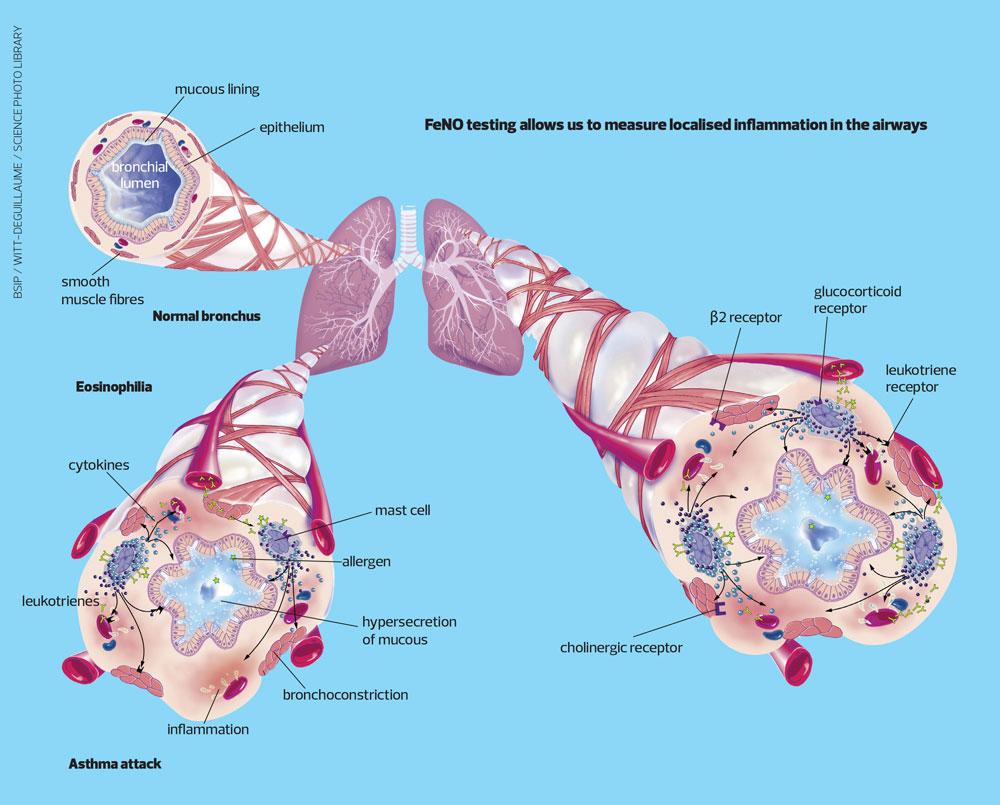
The FeNO test measures the amount of nitric oxide in exhaled breath. A raised level is an indication of active eosinophilic inflammation in the airways, the driving mechanism of which is T-Helper 2 lymphocytes. A raised FeNO level therefore provides us with the ability to identify individuals who will benefit from anti-inflammatory treatment, specifically inhaled corticosteroids.4,5
The test is conducted using a small portable device. The patient blows through a filtered mouthpiece at a controlled rate for 10 seconds. It is not a forced breath. The result is available within a minute. It is a simple test that most people over the age of 5 years can perform quickly with instruction.
CURRENT GUIDELINE RECOMMENDATIONS
It is worth revisiting and understanding the guideline definitions of asthma in order to consider where FeNO is placed in each guideline and if that is still appropriate in rebuilding services, post pandemic.
There is no dispute between the guidelines as to the definition of asthma although the wording may be expressed differently. The British Thoracic Society/Scottish Intercollegiate Guidelines (BTS/SIGN),6 NICE,7 and the Global Initiative for Asthma (GINA)8 all explain that asthma is a chronic inflammatory disorder of the airways and associated with symptoms such as wheeze, cough and shortness of breath, and characterised by variable airway hyperresponsiveness and airflow obstruction.
For many years FeNO has been positioned in the BTS/SIGN recommendations for diagnosis of asthma where there is need for more objective evidence. If, after taking a thorough history and review of the medical notes, the clinician considers there to be an intermediate probability of a diagnosis of asthma, FeNO is one of the potential tests to look for eosinophilic inflammation, alongside blood eosinophils, skin prick testing, or blood IgE.6 Of these tests, though, it is the only one that would demonstrate specific eosinophilic airway inflammation rather than systemic inflammation. The other available tests (reversibility, peak flow charting, challenge testing) would demonstrate variability of airflow obstruction rather than inflammation.
NICE has taken a different approach, recommending objective testing for the diagnosis of asthma in all adults, and in children and young people where there is any diagnostic doubt.7 The recommendations use a combination of spirometry, peak flow and FeNO testing if equipment is available. The testing algorithm follows on from full clinical assessment.
THE ‘ASTHMA TEST’?
It is important to remember there is no single defining feature or symptom of asthma, and there is no definitive ‘asthma test’.8 The diagnosis of asthma should be made through holistic evaluation of the patient symptoms over time. Measurement of lung function should be repeated, as well as evaluation of any response to trials of treatment. A range of tests – a diagnostic toolbox – and observations over a period of time should be used to confirm (or refute) a diagnosis of asthma.9
FeNO does not provide us with a definitive asthma test, but we have a gap in our toolbox if, when we look to diagnose a condition with inflammation at its core, we only look to demonstrate airflow and airflow limitation, or at best look for indications of a generalised inflammatory reaction, when we could be measuring localised inflammation in the airways.
FUNDING
NHS England’s Accelerated Access Collaborative identified FeNO as an item for funding under the Rapid Uptake Products programme in 2020. This programme is designed to support more widespread adoption and dissemination of proven innovations. It identifies products that have NICE approval, that support the NHS Long Term Plan’s key clinical priorities but despite this, have a low uptake.10
Working with the Academic Health Science Networks and using Pathway Transformation Funding, the Accelerated Access Collaborative was able to put together a package that allowed sites to apply for equipment and other costs, but also allowed access to project management, education and peer support networks. Applications have by far outstripped the available funding. This demonstrates not only clinicians’ interest in wanting to add FeNO to their diagnostic toolkit but also that funding and availability of equipment are the biggest potential hurdles to adoption.
FeNO seems to be perceived as an expensive resource to add to available respiratory testing. However, the Scottish consensus statement on the role of FeNO in adult asthma in 2019 found FeNO to be cost effective in diagnosing and managing asthma in a primary care setting, and recommended it should be incorporated into clinical practice.11 This year (2021) Darba et al12 published data from an economic analysis in Sweden that found FeNO to be less costly than comparable methods (spirometry with reversibility testing, methacholine challenge testing, allergy testing, and blood eosinophil count) while providing similar health benefits. This is an interesting consideration for a health system such as the UK where most tests are not associated with cost as there is no direct payment. There is, of course, cost associated with all health care activity even if there is no monetary exchange at the site of clinical activity, so this study gives an insight into the comparative costs.
STRENGTHS OF FeNO TESTING
FeNO is a test that can be quickly and easily added into a consultation. Most patients are able to perform the test with instruction. As it is not a forced manoeuvre and rarely induces cough, it is not considered an aerosol-generating procedure. It is therefore safe to perform the test in the current climate, with usual infection control and prevention measures (a new filter and wiping the outer casing between patients, and PPE as usually worn for face to face consultations).
It is well recognised that asthma is a disease of inflammation, yet we are still shying away from a test that allows us to directly assess any inflammation within the airways. Surrogate markers of blood eosinophils can be affected by other systemic or local influences such as disease or medication, and blood test results may not be found reliably in the notes of younger or otherwise fit people.
LIMITATIONS OF FeNO TESTING
As with all user-dependant testing there will be a small number of patients who will be unable to perform the required manoeuvre despite instruction. In 2007 the author published research where only two subjects in a trial of 37 adults and children were unable to complete testing.13 Since then, the devices have developed and improved, and in my opinion, very few people are unable to yield a result once coached.
Like many other tests, there are some clinical considerations when interpreting the results of FeNO. These are not necessarily a weakness but do cause some anxiety in those unfamiliar with FeNO. Considerations that should be applied when interpreting FeNO values, as they may have a bearing on the result, include:
- Age and gender. Children tend to have lower FeNO levels than adults, and women very slightly lower than men. It is likely this is because FeNO is synthesized from the mucous membrane of the lung and those with a larger surface area (adults >children, men>women) will produce slightly more FeNO.
- Smoking – supresses FeNO by up to 60%
- Rhinovirus infection – increases FeNO by up to 150%, and
- A diet high in nitrates (leafy green vegetables) – increases FeNO by up to 60%, peaking 1-2 hours after consumption
Bjermer et al14 reviewed the evidence around this subject in detail and concluded that most factors only had a small and clinically nonsignificant effect on FeNO. It is important to remember that smoking, for example, also has the potential to effect other respiratory tests such as spirometry.15 As with all tests the results are dependent on the clinical skills of the diagnostician responsible for their interpretation.
TRAINED, COMPETENT AND CONFIDENT
Another point for consideration is the skill of the health care professional undertaking the respiratory diagnosis. For those undertaking spirometry there is a certification and registration process, which although not compulsory, allows employers, patients and inspectors to check that someone performing spirometry is trained and assessed as competent to do so. However, this is just one part of the diagnostic pathway. History taking, clinical examination, performing other tests such as FeNO and peak flow are all vital in making an accurate diagnosis along with the wider holistic skills that are not formally assessed as a whole.
PCRS has produced a guide to the key knowledge, skills and training for clinicians providing respiratory care from standard level through to advanced and expert respiratory care. Fit To Care16 offers a framework for self-assessment and reflection and will help identify gaps in training and competences.
DIAGNOSTIC HUBS
Following publication of the independent report Diagnostics: Recovery and Renewal17 there is work underway to set up community diagnostic hubs. Once set up, these hubs will offer respiratory diagnostics such as spirometry and FeNO testing. However, it is unlikely they will be able to provide the capacity to assess every patient who presents to primary care with a possible diagnosis of asthma or COPD. The decision that has to be made, and in a timely fashion, is how we deliver spirometry to the backlog of patients that has developed over the last year. These patients are waiting for confirmation of a respiratory diagnosis, some will be on incorrect medications, some will be tolerating symptoms. But is this our opportunity to add FeNO into the mix?
CONCLUSION
FeNO testing can be easily incorporated into the respiratory diagnostic pathway as a cost effective investigation of airway inflammation. It forms a part of the diagnostic toolbox for a competent respiratory practitioner.
While the pandemic has sapped much of our energy, it has also allowed us to do things differently, to make changes at pace and to be more nimble at delivering health services. As we adjust to the new normal it is too good an opportunity to just go back to delivering respiratory care as it was before. Despite all of our passion and enthusiasm we weren’t getting it right, not because we weren’t trying, but because the system was weighted against us.
This is our opportunity to Build Back Better. Better might be a better service at practice level with trained, competent confident staff, or better might be in the development of a local diagnostic hub for breathlessness. The vision for these would be for primary care networks to pool respiratory expertise so that patients presenting with breathlessness are seen by a team who are well trained, confident in what they do, and do it regularly. It allows for clinical leadership, mentoring and learning to be built in – and for FeNO to be
a routine part of the diagnostic testing process at PCN level for appropriate patients.
REFERENCES
1. HM Treasury. Build back better: our plan for growth. https://www.gov.uk/government/publications/build-back-better-our-plan-for-growth/build-back-better-our-plan-for-growth-html
2. Royal College of Physicians. Wales primary care clinical audit report 2020. https://www.rcplondon.ac.uk/projects/outputs/wales-primary-care-clinical-audit-report-2020
3. Primary Care Respiratory Society UK, The Association for Respiratory Technology and Physiology. Risk minimisation in spirometry re-start. https://www.pcrs-uk.org/news/new-update-spirometry-guidance
4. Dweik RA, Sorkness RL, Wenzel S, et al. Use of exhaled nitric oxide measurement to identify a reactive, at-risk phenotype among patients with asthma. Am J Respir Crit Care Med 2010;181:1033-1041
5. Smith AD, Cowan JO, Brassett KP, et al. Exhaled nitric oxide: a predictor of steroid response. Am J Respir Crit Care Med 2005;172;453-459
6. British Thoracic Society. BTS/SIGN British Guideline on the Management of Asthma. https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/
7. NICE NG80. Asthma: diagnosis, monitoring and chronic management. https://www.nice.org.uk/guidance/ng80
8. GINA. Global strategy for asthma management and prevention (2021 update). https://ginasthma.org/wp-content/uploads/2021/05/GINA-Main-Report-2021-V2-WMS.pdf
9. Stonham C, Baxter N. FeNO testing for asthma diagnosis – A PCRS Consensus; 2019. https://www.pcrs-uk.org/sites/pcrs-uk.org/files/pcru/articles/2019-Autumn-Issue-18-FeNo-testing-asthma-diagnosis.pdf
10. NHS England. NHS Long Term Plan. https://www.longtermplan.nhs.uk
11. RuiWenKuo C, Spears M, Haughney J, et al. Scottish consensus statement on the role of FeNO in adult asthma. Resp Med 2019;155:54-57
12. Darba J, Ascanoo M, Syk J, Alving K. Economic evaluation of the use of FeNO for the diagnosis and management of asthma patients in primary care in Sweden. ClinicoEconomics and Outcomes Res 2021;13:289-297
13. Gruffydd-Jones K, Ward S, StonhamC, et al. The use of exhaled nitric oxide monitoring in primary care asthma clinics: a pilot study. Prim Care Resp Journ 2007; 16:349-356. https://www.nature.com/articles/pcrj200776
14. Bjermer L, Alving K, Diamant Z, et al. Current evidence and future research needs for FeNO measurement in respiratory diseases. Resp Med 2014;108(6): 830-841
15. Primary Care Commissioning. A guide to performing quality assured diagnostic spirometry; 2013. https://www.brit-thoracic.org.uk/media/70454/spirometry_e-guide_2013.pdf
16. Lawler R. Fit To Care: key knowledge skills and training for clinicians providing respiratory care; 2020. https://www.pcrs-uk.org/sites/pcrs-uk.org/files/resources/2019-FitToCare.pdf
17. NHS England. Diagnostics: Recovery and Renewal; 2021. https://www.england.nhs.uk/wp-content/uploads/2020/11/diagnostics-recovery-and-renewal-independent-review-of-diagnostic-services-for-nhs-england-2.pdf