Asthma for the 21st century
Beverley Bostock-Cox
Beverley Bostock-Cox
RGN MSc MA QN
Nurse Practitioner Mann Cottage Surgery Moreton in Marsh
Education Lead Education for Health, Warwick
Why has the National Review of Asthma Deaths made little apparent difference to the standard of care of people with asthma? We review the findings and examine latest developments to see if they can help to address the issues NRAD revealed
In 2014 the findings of the National Review of Asthma Deaths (NRAD) were published.1 The aim of the publication, as the title made clear, was to identify ‘Why asthma still kills’ in order to address any gaps in care, from diagnosing and managing stable asthma through to preventing, identifying and treating asthma attacks using appropriate treatment and supported self-management. Yet recent statistics from a survey by Asthma UK, suggest that asthma remains a challenge with significant numbers of people having symptoms which regularly impact on their day to day life.2
In this article, we review the findings of the NRAD report and the Asthma UK survey and consider why the NRAD report has not had the anticipated effect on asthma diagnosis, management and death rates. We also debate whether new research, technology and treatments from the past five years can help to address these issues.
THE NATIONAL REVIEW OF ASTHMA DEATHS
NRAD was not set up to count asthma deaths or provide statistics on the number of people dying from asthma, but was primarily an investigation into the causes of those deaths. As asthma is, for the most part, a treatable condition, any death is a tragedy. This begs the question: why are people still dying and what can be done about it?
Some of the key messages from NRAD were that people who died from asthma were more likely to overuse their blue reliever inhalers and underuse inhaled corticosteroids. They were also less likely to attend for review appointments, making it harder for health care professionals to engage in discussion about these potentially risky behaviours. It was found that basic asthma care was lacking, from diagnosis through to prescribing in stable asthma and managing acute asthma attacks. People with asthma were also not supported to self-manage effectively, resulting in too many people (especially children) dying before reaching hospital. This suggested that people did not understand how serious an asthma attack can be or the importance of seeking help early on in the attack.
THE REALITY OF ASTHMA CARE IN THE UK
Asthma UK’s annual asthma survey the reality of asthma care in the UK, published earlier this year, compared the care people were receiving in practice with the recommendations made in the latest NICE guidance.3 It is perhaps worth stating that the NICE guidelines did not receive universal praise when they were published in 2017. There were key contrasts between NICE and the guidelines from the British Thoracic Society/Scottish Intercollegiate Guidelines Network (BTS/SIGN)4 with respect to asthma diagnosis and treatment. NICE did not include advice on managing acute asthma either. However, there is common ground regarding the areas highlighted in the report for NICE, BTS/SIGN and the latest Global Initiative for Asthma (GINA) guidelines.5
It should be remembered that health surveys will be completed by a self-selecting group and may be affected by response bias, whereby certain patient groups will be more or less likely to respond to a survey based on how the survey is carried out (online, by phone, mail or face to face), socioeconomic status, cultural differences, language barriers or disability, for example.6 Just over 10,000 people responded to the survey, out of a reported asthma prevalence of around 3.24 million people, so in many ways it would be risky to make assumptions about asthma care based on the experiences of 0.003% of the affected population. If three out of five people (in the survey) are not getting basic asthma care, that’s still only 0.0018% of the asthma population. However, in reality these findings are likely to reflect a bigger picture of sub-optimal care in too many cases, so the survey highlighted some interesting findings that clinicians working in asthma care may do well to reflect upon.
- Three out of five people didn’t receive basic care
- Young people receive the worst level of basic care
- People may be suffering more asthma attacks than previously estimated (two attacks per year, compared with 0.57 calculated from 2013 surveillance data)
- Follow-up after emergency care is still being missed.
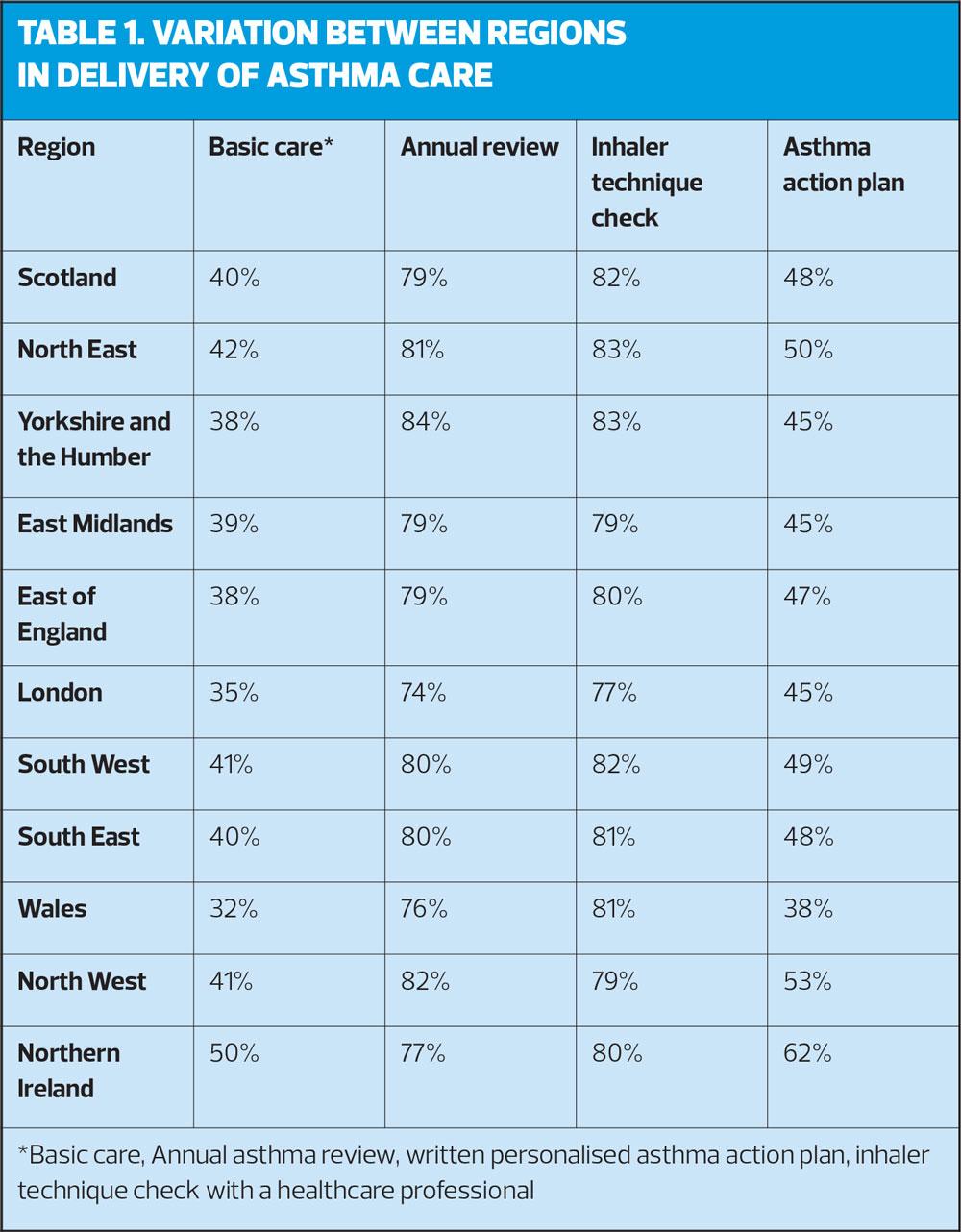
Widespread variation was seen throughout the UK in the percentage of people receiving basic care. London and Wales were identified as areas which fared the worst in the survey (Table 1).
HOW CAN WE IMPLEMENT STRATEGIES TO ADDRESS THESE ISSUES?
So how can general practice nurses (GPNs) ensure that the messages from NRAD and the Asthma UK survey are acted upon? Some reflection on current service provision is required and GPNs need to think what they can do personally in order to improve standards. The NRAD authors made recommendations to address some of the gaps. They suggested that every practice should have an asthma lead and that all practice staff delivering asthma care should be trained and competent. Does your practice have an asthma lead? This should be someone who is appropriately trained, up to date and competent to lead asthma care in the practice, and liaise with the multi-disciplinary team where required. For some time, nurses have taken the lead in respiratory care provision in general practice so it is entirely right that nurses should consider being the asthma lead for the practice, but they should be supported to maintain their competence with protected time to access up to date information and training.
ASSESSING INHALER USE
Recognising that people who die from asthma were more likely to overuse their blue reliever inhalers, consideration should be given to ensuring that reliever inhalers are only issued as acute prescriptions. Good asthma control should mean that only one or two reliever inhalers are required per year so anyone using more than this should be considered for review, although for pragmatic reasons the limit is often set at six.* It was when people were using six or more relievers per year that asthma deaths were seen to rise in NRAD, so this is a suitable initial benchmark for poor control, although BTS/SIGN suggests that people using 12 or more inhalers per year should be considered for urgent review.4 The underuse of inhaled corticosteroids has been linked to asthma exacerbations and deaths.4 This is unsurprising when considering that asthma is an inflammatory disease and that inhaled corticosteroids (ICS) have an anti-inflammatory action. People with asthma (or parents of children with asthma) may fear the negative impact of taking a daily ICS so need to have a clear explanation of the way in which inflammatory changes can impact on lung health and how the ICS will support healthy lung function.
*The recently published BTS/SIGN guideline suggests that clinicians should consider ‘stepping up’ treatment for anyone using more than 3 doses of a short-acting bronchodilator per week
ASTHMA REVIEWS FOR THE 21ST CENTURY
Asthma UK also makes key policy recommendations, including the need to reach more people for asthma reviews (making text message reminders standard practice) and the provision of more written asthma action plans. They also state that not enough people are getting a review within 48 hours of an asthma attack, something which is written into the Asthma Quality Standard.7 GPNs should ensure that there is effective communication and systems between primary and secondary care to facilitate these swift reviews.
People who died with asthma were also less likely to attend for review appointments, making it harder for health care professionals to engage in discussion about these potentially risky behaviours. As a result, GPNs need to consider newer ways of engaging with people that make a trip to the surgery for an asthma review more obviously worthwhile. If people feel that they are attending predominately so we can tick our boxes, they are unlikely to be prepared to take time out (potentially losing pay or school study time in the process) to attend.
Investment (and not necessarily financial) should be made into new ways of working, including supporting people to implement motivational interviewing techniques into their general practice consultations – something which is entirely possible according to Dr Lee David, author of ‘Using CBT in General Practice: The 10 Minute CBT Handbook’.8 Group consultations are another way of reaching more people in a novel but effective way.9 Our reluctance to engage through telephone consultations or other digital media needs to be put aside in order to embrace technology and today’s ‘virtual’ world.
SCHOOL-BASED CARE
There should be better liaison with schools as this has been shown to improve asthma clinic attendance from 51% to 91%.10,11 One way of developing links with schools could be to introduce them to the Supporting Children’s Health website where non-clinicians can learn about asthma care. This can be accessed here: https://sch.educationforhealth.org/wp/ Maybe a school-based group consultation for people with asthma could work? Or a work-based one for that 18-29 age group where they are finding it more of a challenge to come into surgery. We need to think differently.
APPROPRIATE INHALER CHOICES
Asthma UK reported that deaths from asthma in the UK remain higher than in the rest of Europe, in spite of the fact that NHS asthma reviews are free for all. This is a real conundrum. Why do we do so badly? Europe prescribes more dry powder inhalers than the UK and these may be associated with better outcomes,11 so recent guidance from NICE about prioritising DPIs might help, even though the guidance was based on environmental concerns rather than asthma control issues.12 Nonetheless, the most important consideration is to match the inhaler to the individual. Inhaler technique is fundamental to good asthma control. Online resources such as the Asthma UK inhaler videos https://www.asthma.org.uk/advice/inhaler-videos/ or the RightBreathe website https://www.rightbreathe.com/ and app provide further support to clinicians and patients, as they can be shown during the review and then used at home to support ongoing correct technique. ‘Smart’ inhalers (confusingly named as they are often mixed up with the ‘maintenance and reliever or MART’ approach to asthma management) could also be the future of asthma care. Smart inhalers are explained and the rationale given for their use in a 2017 article on the Asthma UK website.14
Acute asthma
NRAD said that people with asthma were not supported to self-manage effectively, resulting in too many people (especially children) dying before reaching hospital.1 The severity of an asthma attack can be quickly assessed using the SHARP tool, and comparing results with expected values for each individual.4
SHARP
- SATs
- Heart rate
- Ability to talk in sentences/accessory muscle use
- Respiratory rate
- Peak flow
Once the assessment has been carried out, management can follow the ABCDE mnemonic:
ABCDE
- Assess for severity and act accordingly
- Bronchodilate
- Corticosteroids
- Document all findings
- Evaluate throughout
PATIENT INVOLVEMENT
So where does patient responsibility come into this debate? The Asthma UK report2 repeatedly advises patients to ‘demand’ better care but I may not be alone in feeling that this suggests that some clinicians are deliberately underperforming. Although this may be so (knowing or unknowing incompetence being the problem), in reality many nurses report patient apathy when it comes to taking regular inhalers, engaging with the self-management plans or stopping smoking. Is it always a reflection on the clinician if someone has an asthma attack? Similarly, is it not at least partly understandable that people with a long term condition should be reluctant to carry medication and an asthma action plan with them wherever they go, so they are constantly reminded of their ‘invalid’ status? Rather than written asthma action plans (the holy cow of asthma care) would it not be better to just ask people three simple questions in their asthma review:
- What does good asthma control feel like to you?
- When do you know that your asthma control is deteriorating?
- What do you do about it?
Asking these three questions would be a start to encouraging ownership of the condition and a recognition of what to do when, in order to avoid a hospital admission or even an asthma death. Could we introduce people with asthma and their carers to the SHARP mnemonic to make it easier for patients to self-assess?
Digital technology may enhance the way in which people with asthma (and other long term conditions) self-manage. As a result, Asthma UK has developed a 12 week online support programme for people with asthma which can be accessed here: https://www.asthma.org.uk/for-professionals/professionals/12wkasp-hcps/
However, for some people 12 weeks may feel like a big commitment so they may prefer to use other digital technology, such as the mymhealth® asthma app available from https://mymhealth.com/myasthma, to support self-management, especially as it is the 18-29 age group who seem to be most affected by the poor asthma management, according to Asthma UK. Some primary care organisations have made these available to practices through a licensing scheme, but individuals can purchase lifetime access to the app for £39.99. The Asthma UK Facebook page can also help to support people who have asthma but can also be educational for health care professionals who can hear what people with asthma are saying about the asthma care they are currently getting. You can find the page at www.facebook.com/asthmauk
If people in the 18-29 age group are more than twice as likely to need emergency care as older people over 60, is that because they are too busy living their life to (potentially) save it, by attending their review? Are asthma costs a bigger concern for young people? The over 60s and the under 18s both do better with regard to their asthma control so why is that? Does the disease change or do their priorities?
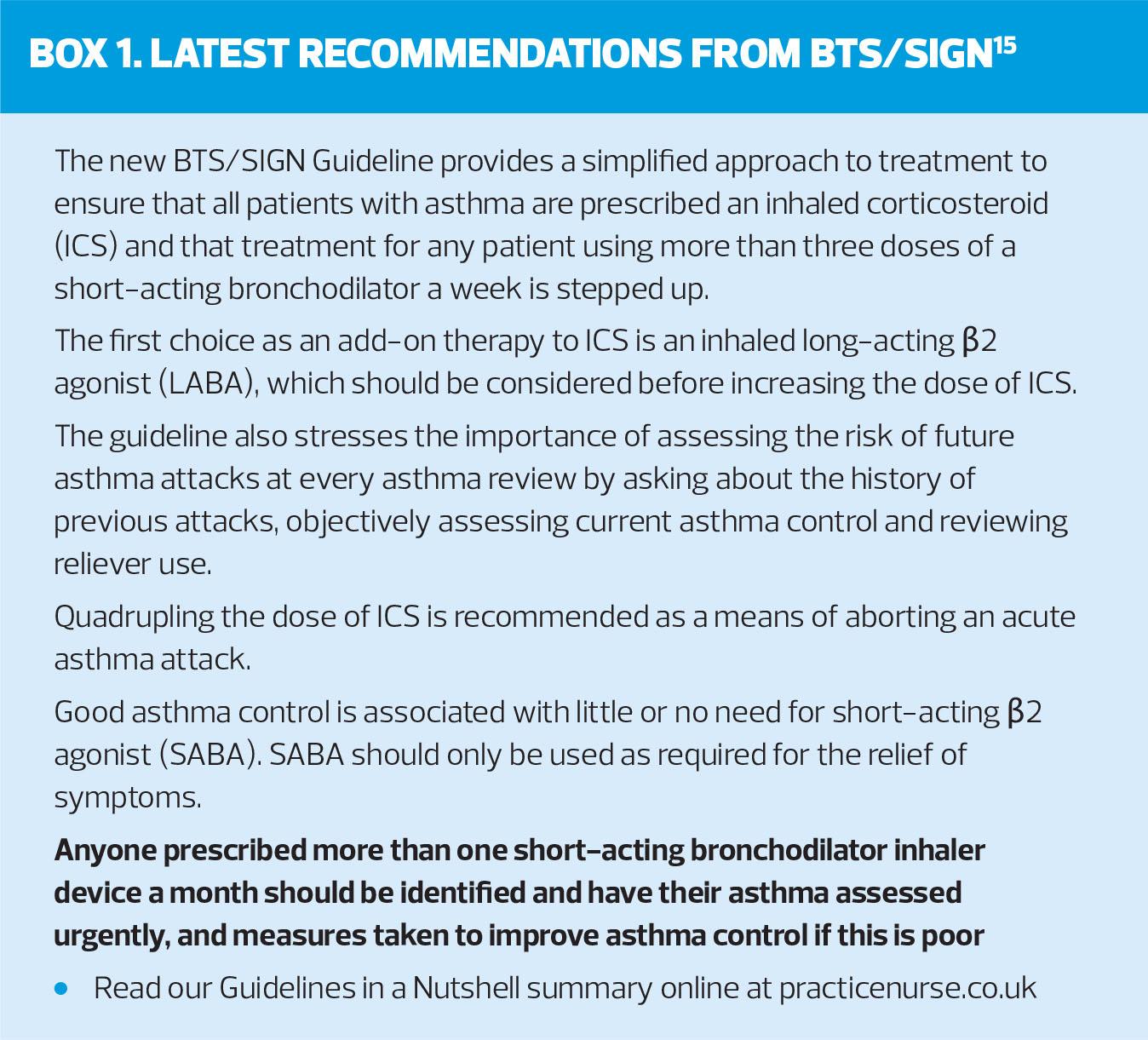
WHAT’S NEW IN ASTHMA WHICH MIGHT HELP MAKE A DIFFERENCE?
New treatment options are available since the NRAD report was published and clinicians need to support people with asthma to work out the inhaler, regime and management strategy that will work best for them. Relvar® offers a once daily ICS/LABA which may, for some people, improve adherence; the long acting muscarinic antagonist (LAMA) Spiriva® has now been licensed to treat asthma in children age 6 and over, Flutiform® is now available as a breath triggered device (the K-Haler®) and Symbicort® maintenance and reliever therapy (SMART) is licensed from age 12 years. Furthermore, the recent GINA guidelines endorsed the (unlicensed) use of formoterol-containing ICS/LABA therapy on an ‘as required’ basis. Triple therapies for asthma will also be available soon. Asthma UK is also campaigning to end prescription charges for people with asthma – details are available here: https://www.asthma.org.uk/support-us/campaigns/our-policy-work/prescription-charges/. Finally, guideline-based care is important but it needs to start with the guideline, so an evidence based approach with one national guideline from BTS/SIGN with NICE is eagerly anticipated (See Box 1).15
CONCLUSION
Asthma is a treatable condition and deaths are largely avoidable, as demonstrated in the NRAD report. The recent Asthma UK survey reminds us that there is still a great deal of room for improvement in asthma care, although clinicians should be aware that the survey reflected the experiences of a small proportion of the asthma population in the UK. Nonetheless, the survey is a reminder of the fact that people are suffering needlessly with uncontrolled asthma symptoms and that all avenues should be explored to make asthma care simple, structured and accessible for all.
REFERENCES
1. Royal College of Physicians. Why Asthma Still Kills: The National Review of Asthma Deaths (NRAD), 2014 https://www.asthma.org.uk/globalassets/campaigns/nrad-full-report.pdf
2. Asthma UK. The reality of asthma care in the UK, 2019 https://www.asthma.org.uk/578f5bcf/globalassets/get-involved/external-affairs-campaigns/publications/annual-asthma-care-survey/annual-asthma-survey-2018/asthmauk-annual-asthma-survey-2018-v7.pdf
3. NICE NG80. Asthma: diagnosis, monitoring and chronic asthma management, 2017 https://www.nice.org.uk/guidance/ng80
4. British Thoracic Society/Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma, 2016 https://www.brit-thoracic.org.uk/document-library/clinical-information/asthma/btssign- asthma-guideline-2016/
5. Global Initiative for Asthma. Asthma Management and prevention, 2019 https://ginasthma.org/wp-content/uploads/2019/04/GINA-2019-main-Pocket-Guide-wms.pdf
6. Heath S. What Is Non-Response Bias in Patient Satisfaction, CAHPS Surveys? Patient Engagement Hit, 05 February 2019 https://patientengagementhit.com/news/what-is-non-response-bias-in-patient-satisfaction-cahps-surveys
7. NICE QS25. Asthma Quality Standard, 2018 https://www.nice.org.uk/guidance/qs25
8. David L. Using CBT in General Practice, second edition: The 10 Minute CBT Handbook. Banbury, Oxon; Scion Publishing: 2013
9. Bostock-Cox B, Brady L, Hodgson EK. Group consultations: the why and the how. Practice Nurse 2019;49(04):34-37. http://www.practicenurse.co.uk/index.php?p1=articles&p2=1864
10. Salisbury C, Francis C, Rogers C, et al. A randomised controlled trial of clinics in secondary schools for adolescents with asthma. Br J Gen Pract 2002;52(485):988-96.
11. Bostock-Cox B. Acute asthma attacks in the school setting: Diagnosis and prevention. Brit J School Nursing 2018;13:10
https://doi.org/10.12968/bjsn.2018.13.10.479
12. Ramadan WH, Sarkis AT. Patterns of use of dry powder inhalers versus pressurized metered-dose inhalers devices in adult patients with chronic obstructive pulmonary disease or asthma: An observational comparative study. Chronic Respiratory Disease 2017;14(3):309–320. doi:10.1177/1479972316687209
13. NICE. NICE encourages use of greener asthma inhalers (press release), 2019 https://www.nice.org.uk/news/article/nice-encourages-use-of-greener-asthma-inhalers
14. Asthma UK. Smart asthma, 2017 https://www.asthma.org.uk/smartasthma
15. BTS/SIGN. British Guideline on the Management of Asthma, 2019 https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/